Speech therapy, also known as speech-language pathology, is a specialized field of healthcare aimed at diagnosing and treating communication disorders.
It addresses various challenges, such as articulation difficulties, language delays, voice disorders, fluency issues (stuttering), and more. Therefore, a speech-language pathologist (SLP) aims to improve speech clarity, language comprehension, expressive communication, and overall communication skills.
To administer the appropriate care, they must track the progress of any medical interventions and plan how to provide patient-centered care. The most efficient tools for documenting patients’ progress and therapy sessions are SOAP notes, alternatively known as progress notes.
This article will discuss the information you should include in a SOAP note as a speech therapist. This is achieved by analyzing the different components of the standard format of such a document. Lastly, it will provide tips for improving your documentation. You can use the templates we have provided to create the note. The templates are free for download and are predesigned to make them convenient for your use.
What is a Speech Therapy SOAP Note?
The term “SOAP” is an acronym for Subjective, Objective, Assessment, and Plan. In speech therapy, SOAP notes serve as a structured method for documenting patient encounters and treatment sessions.
The Subjective component documents information the patient or caregiver provides, such as complaints, experiences, and progress. Then, the Objective component documents data collected during the therapy session (e.g., test results, measurements, clinical observations). Subsequently, the Assessment component outlines your analysis and interpretation of the available data to identify the patient’s progress and changes in their condition.
Lastly, based on your professional evaluation, the Plan component outlines the personalized treatment strategy that will be implemented, including its future goals and interventions. The notes aid in tracking patient progress, facilitating effective communication among healthcare professionals, and ensuring comprehensive and consistent patient care.
Components of a SOAP Note for Speech Therapy
The note format helps you maintain accurate and organized records of your patients. It also facilitates communication with other healthcare professionals and ensures that therapy is evidence-based and tailored to each patient’s needs. While the information recorded in the note will vary with the circumstances, the basic components remain the same.
Below is a comprehensive examination of the essence of each component of a SOAP note. Examples have also been provided to illustrate the type of information you should record under each section of the note for speech therapy:
The header section is typically placed at the top of the note and serves as a quick reference to identify the patient, therapist, and session details. Under this section, start by recording the date, time of the session, and name of the facility to create a chronological record of the patient’s treatment.
Then, indicate the full name, age, and gender of the patient, followed by your name and credentials or designation. This information ensures proper documentation and enables easy retrieval of patient records for future reference or communication with other medical providers involved in the patient’s care.
Subjective (S)
In the subjective section, you should record the patient’s self-reported or caregiver-reported information. This includes the chief complaint, relevant personal experiences, medical history, and any subjective symptoms or concerns related to speech or communication challenges. It may also contain information about the patient’s daily activities, response to previous interventions, and their perception of progress since the last session. This information is needed to provide context to the patient’s communication challenges.
EXAMPLE
- The patient reports difficulty pronouncing certain sounds and feels frustrated during conversations.
- The caregiver mentions an improvement in their communication skills when using visual aids.
Objective (O)
Use this section to record measurable (qualitative and quantifiable) information. This includes test results, clinical observation of the patient’s communication skills, and any relevant measurements taken during the session. This information is needed to assess the patient’s speech or communication abilities and formulate viable and suitable treatment plans.
EXAMPLE
- During articulation exercises, the patient had difficulty producing the /r/ sound correctly in initial and medial positions.
- The patient scored 75% accuracy in following multi-step verbal directions during a language assessment.
Assessment (A)
The assessment section documents your professional interpretation and analysis of the subjective and objective data. It provides an overall impression of the patient’s current communication skills, areas of strengths and weaknesses, and any relevant diagnoses or clinical findings. The assessment may lead to identifying a diagnosis or determining the effectiveness of the previous treatment plan.
EXAMPLE
- The patient’s articulation difficulties may be related to a phonological processing disorder.
- The patient’s receptive language skills have improved, but expressive language delays are still evident.
Plan (P)
In the plan section of SOAP note, you should outline the next steps in the patient’s treatment based on the assessment. This includes setting specific goals, choosing appropriate therapy techniques, and discussing any changes to the treatment plan. It should be a detailed roadmap for future sessions and should be tailored to the patient’s unique needs, progress, and objectives.
EXAMPLE
- Goals for the next sessions include improving the production of the /r/ sound in all word positions.
- Introduce visual supports and communication strategies to enhance the patient’s expressive language skills.
- Schedule weekly 45-minute therapy sessions for the next six weeks to work on targeted speech and language goals.
The footer section typically includes your signature. Your signature is meant to authenticate the information documented in the note and confirm its accuracy. It also confirms that you have reviewed and agree with the information recorded in the note. The signature enhances the legality of the note and ensures that you take responsibility for its content.
SOAP Note Examples and Free Templates
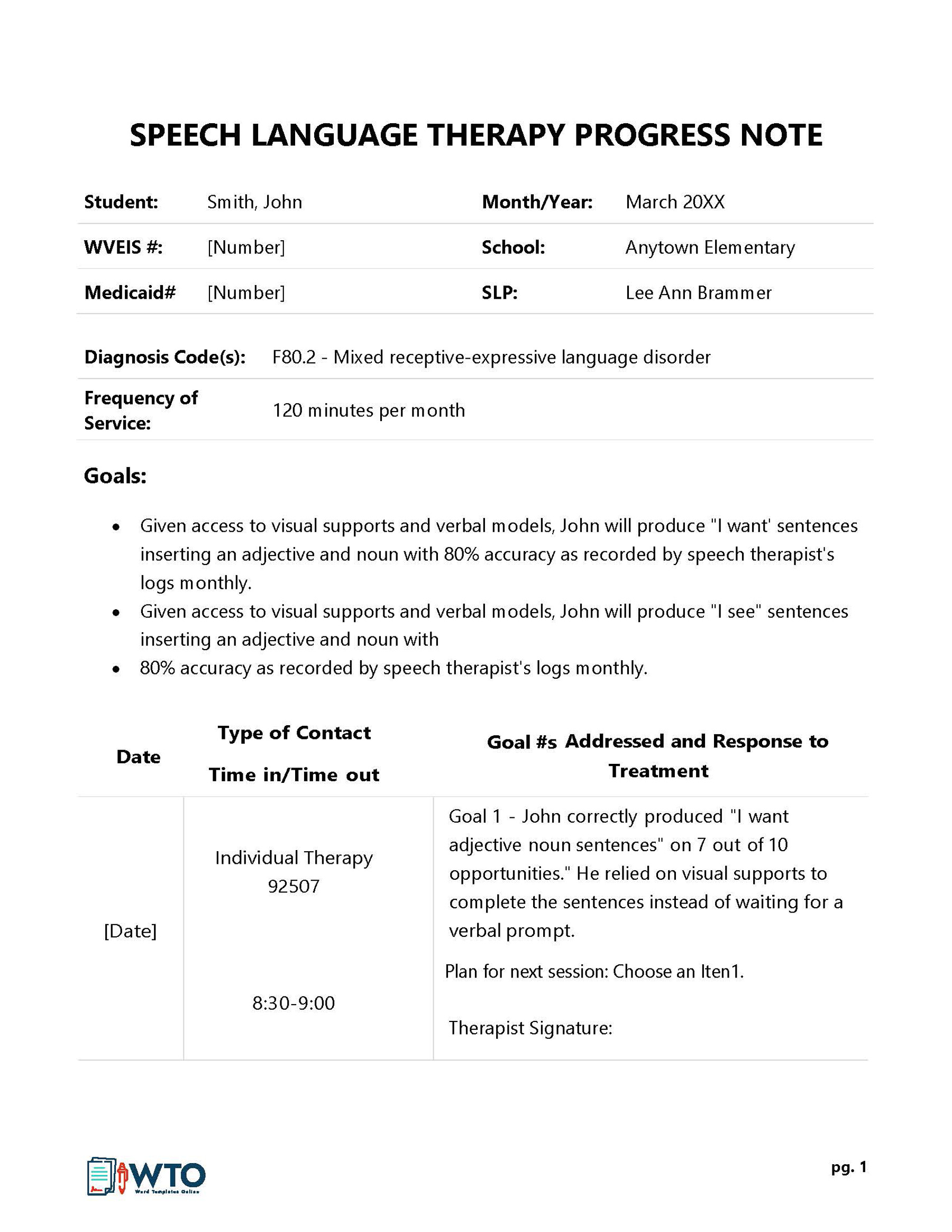
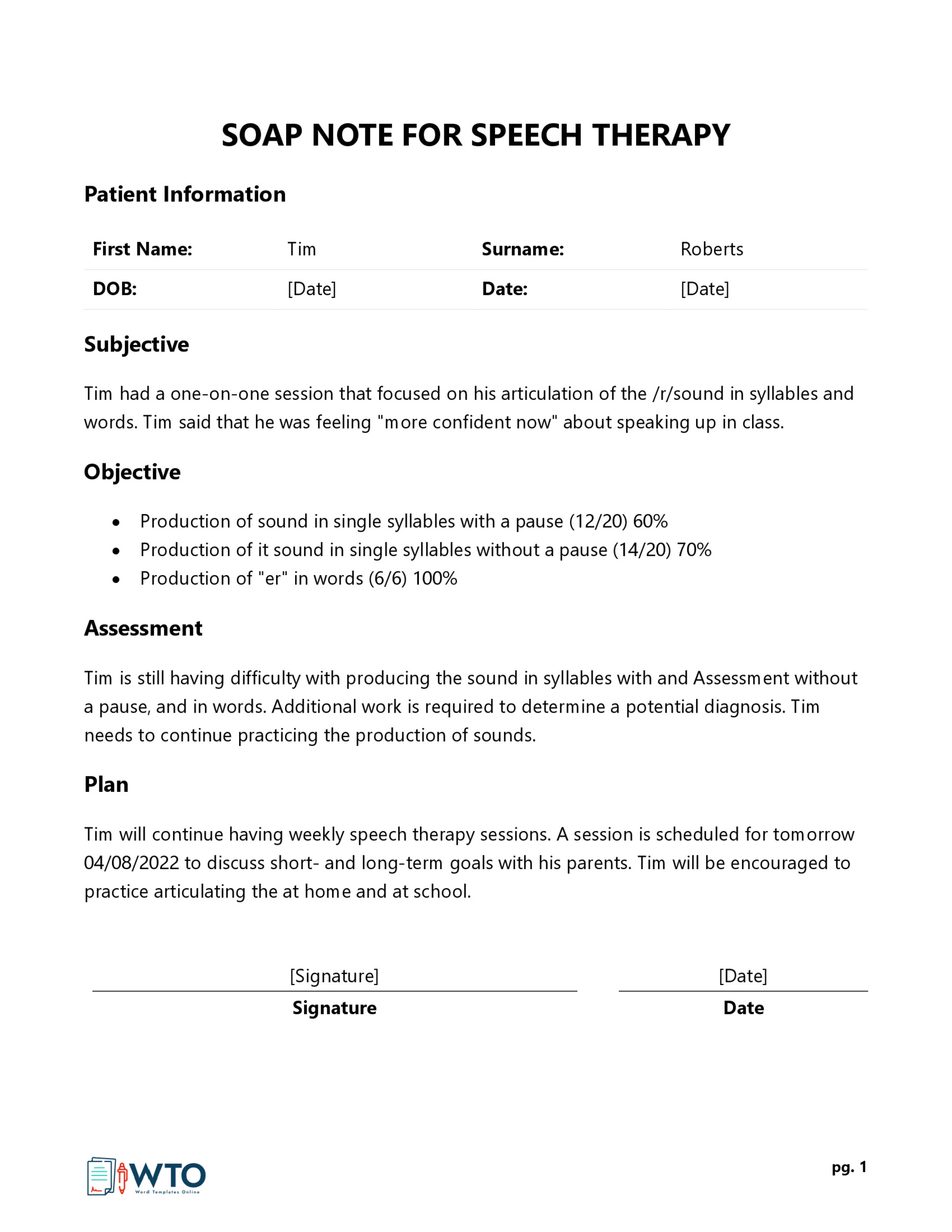
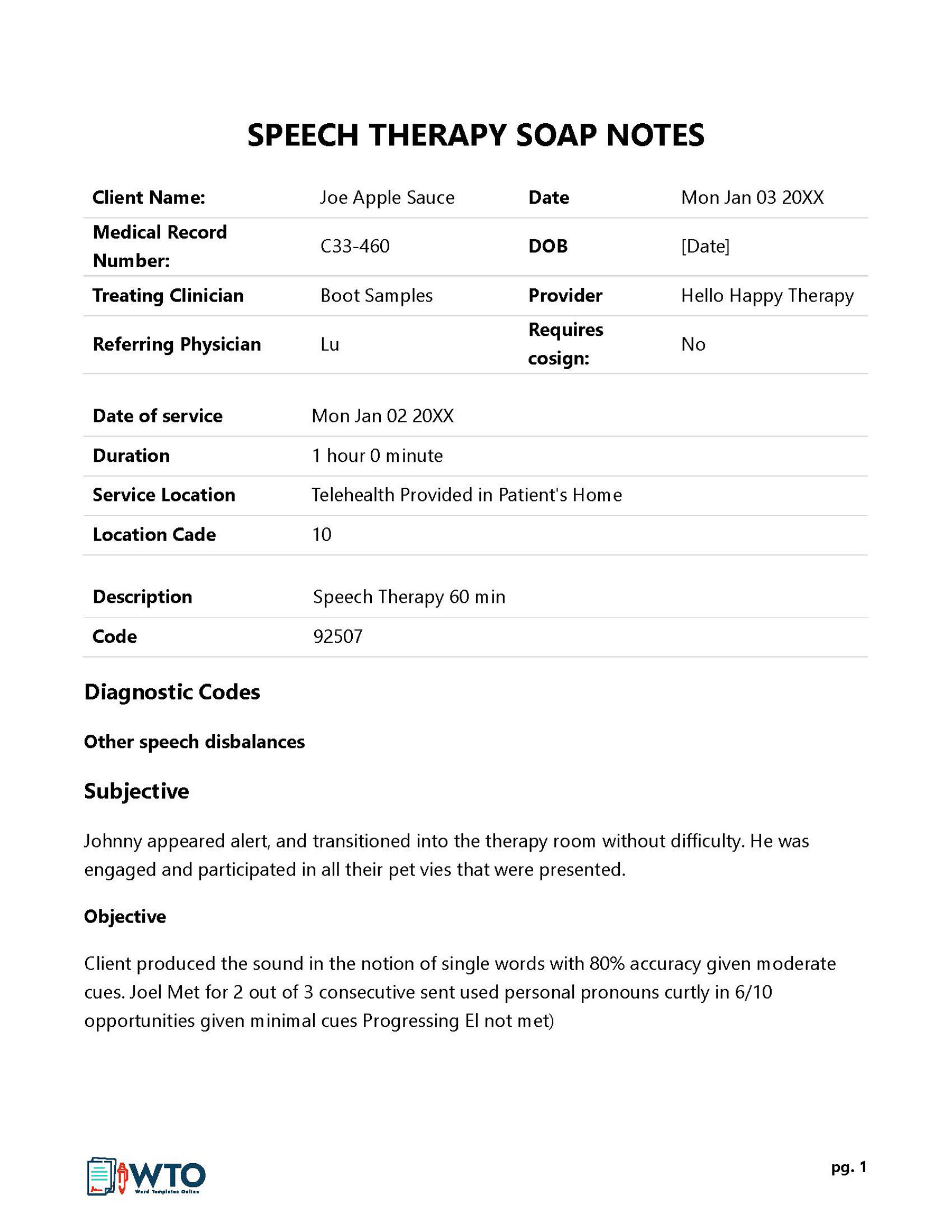
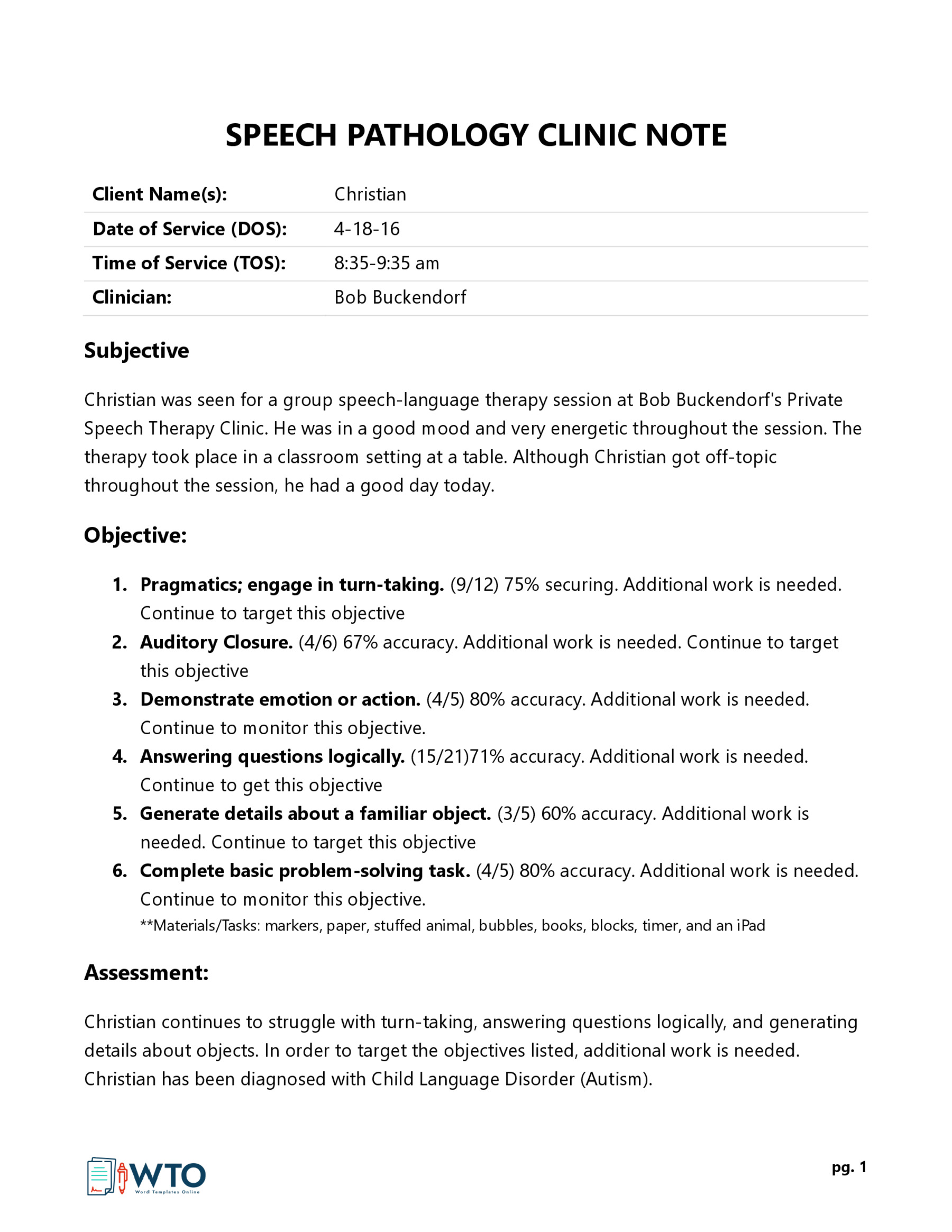
Given below are the speech therapy SOAP note templates:
Best Practices for Efficient Documentation of Speech Therapy SOAP Notes
Efficient and accurate speech therapy documentation is crucial for maintaining high-quality patient care. This is because it facilitates communication among healthcare professionals and ensures you adhere to professional standards.
Here are some best practices to ensure efficient documentation:
Clear and concise language
Write in a clear and simple manner, using professional terminology when appropriate. Avoid unnecessary jargon or abbreviations that may not be very clear to others. This ensures that the content is understandable and lowers the chances of misinterpretation by other professionals involved.
Structured format
Use a systematic structure to record information in the SOAP note. This ensures consistency in documentation and makes it easier to find specific information when needed. Also, it facilitates uniformity and adds a professional look to the documentation within your facility.
HIPAA compliance and patient privacy
Maintain patient confidentiality and abide by HIPAA (Health Insurance Portability and Accountability Act) regulations when documenting sensitive information. So, be selective about the personal information you collect and limit access to the patient’s records to authorized personnel only.
Use a template
Establish a consistent and well-organized template for SOAP Notes. This ensures that all necessary sections are included. A template also provides a structured framework that allows you to organize your notes consistently. It also ensures that the notes are easily accessible during and after the therapy session to track the patient’s progress more precisely.
Regular review and updates
Take the time to review the notes for accuracy, completeness, and adherence to professional standards before signing and finalizing them. Also, regularly review and update the patient’s progress. Document any new and modified interventions to keep the documentation accurate and up-to-date.
Conclusion
SOAP notes in speech therapy help maintain accurate and organized records of patient care. They also facilitate effective communication between healthcare providers and ensure that the therapy provided is evidence-based and tailored to each patient’s needs. These notes are essential for tracking progress over time, making informed treatment decisions, and providing high-quality patient-centered care.
You can utilize a template to create these notes as a speech-language therapist. A template offers a structured format for organizing the patient’s diagnosis and treatment details. This way, you are able to document such information for multiple patients with ease consistently.




