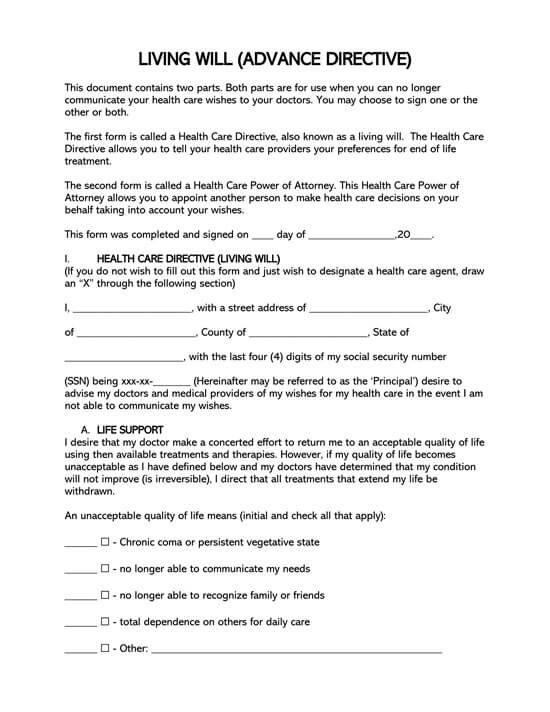
A living will is a legally binding medical document or form that grants individuals the right to state their end-of-life treatment and care.
The document outlines directives for a medical health care provider if an individual falls into a coma or is unresponsive.
This form is a medical power of attorney, which authorizes an agent to make medical decisions when or if a patient is left incapacitated by disease, accident, or surgery. The document does, however, lose its bearing after death.
It is also known as:
- A health care directive
- Advance medical directive
- An advance healthcare directive.
Free Living Will Forms & Templates
Standard form
By states
Living Will- an Overview
Following are a few basic things to know about a Living Will:
What a living will states?
The scope of the document is in force as long as the individual concerned is still alive. It ceases to hold after the death of the affected individual. The document states the following:
- In case you intend to use any sophisticated medical equipment like ventilators, dialysis machines, and so on to maintain you alive.
- Instructions prohibiting the use of CPR in the event of heartbeat or breathing problems.
- Whether you prefer liquid or fluids intakes or food tube feeding if you cannot eat normally.
- In case you desire treatment for nausea, pain, and other associated symptoms but cannot make this decision independently at that time.
- Whether you intend to have your organs or other bodily tissues donated after your death.
The living will come in diverse shades and forms. They may, however, be categorized into three main kinds namely:
- A ‘medical power of attorney’ – This one delegates the decision-making to a third party, typically your own attorney.
- POLST (Physician Orders for Life-Sustaining Treatment) – In this instance, the decision is triggered by a healthcare practitioner rather than the patient himself. It achieves the same end though.
- ‘Do not Resuscitate’ (DNR) Orders – The aim of this specific document is to restrain the physician from resuscitating the patient if he happens to experience breathing or blood circulatory issues.
Purpose of a living will
The living will document serves as an informative backbone for the doctor, directing them on medical do’s and don’ts for patients who cannot communicate their own medical decisions.
The document can come in handy for situations that require decision for patients, such as:
- A patient on life support
- A patient confined a vegetative state
- A patient in need of tube-feeding
- A patient in a mechanical ventilation
- A patient in need of dialysis
- A patient who wishes to donate their organs
There should be no confusion between a living will and a last will and testament, which deals with the distribution of property and other items belonging to the diseased. The living will is also different from a do-not-resuscitate form which prohibits a physician from providing life-saving treatment like CPR.
Possible end-of-life care decisions to discuss in your living will
There are a number of possible end-of-life care decisions which you may discuss in your living will. Below are but a few of them:
- Cardiopulmonary Resuscitation: Cardiopulmonary resuscitation is an emergency medical procedure that endeavors to preserve the functioning of the brain until such a time that further medical care may be conducted. It incorporates chest compressions often and artificial ventilation.
- Mechanical Ventilation: In the unlikely event of not being able to breathe, mechanical ventilation is invoked. It makes use of mechanical approaches to yield breathing power. The concept is also called assisted breathing.
- Tube Feeding: For those who cannot eat normally, tube feeding comes in to provide the necessary assistance. Here, a tube is used to channel usually liquid foods to the body’s cardiovascular system directly.
- Dialysis: Many people experience kidney failures as they age. This is where kidney dialysis comes in. It plays the same roles as a kidney i.e. purifying the blood, filter out impurities, and maintain your blood spotlessly clean.
- Antibiotics or Antiretroviral Medication: Most terminal illnesses are caused by bacteria and viruses. These require powerful antibiotics and antiretroviral medications. You may choose to have your doctor not administer these to you if you happen to find yourself in need of them.
- Comfort (Palliative) Care: Some terminal conditions require extra comfort over and above the normal treatment approaches. These are referred to as comfort or palliative care. You may yet again choose to relinquish these from your terminal healthcare.
- Organ and Tissue Donation: Would you wish to have your tissues or organs donated after your passing? If you desire so, this document accords you a good chance to do just that. You may state the organ you want to donate to a third party.
- Complete Body Donation: Other than specific portions of your body, you may as well recommend that your whole body be donated to a medical research firm for the purposes of advancing the medical field.
Differences between a living will and medical power of attorney
A living will differ from the medical power of attorney in that it is drafted and worded expressly by you. The latter may be drafted by a third party, typically a legal agent who is familiar with your health and has some permission from you too. Be sure to confirm that he is in your best interest before delegating this responsibility to him though.
Writing a Living Will
An individual can draft their living will in a day without an attorney or the inconvenience of having it filed in a government office. This makes the process fast and easy as a patient requires it to input their end-of-life treatment options and have it signed before a witness or a notary public, depending on the state.
Crafting it involve the following:
Select the treatment options
At this stage of the crafting process, the patient is encouraged to take a step back and contemplate the course of action they would want to be taken in the event of:
- A coma
- Vegetative state
- Incapacitation
- Dementia
- Severe Alzheimer’s Disease
Deciding the course of action to be taken regarding an individual’s life cannot be quickly done alone. It is recommended that such critical decisions are made with the family to prepare them for any life-threatening event. An individual should decide if the medical personnel should do everything they can to save their lives or allow a peaceful death if they cannot independently breathe or eat. The final decision should be written in this document to act as a reference point for medical health care providers treating the patient.
Decide the end-of-life decisions
Any additional information like the carrying out of last religious rites by a priest or Sheikh should be part of this document. Specific funeral plans such as wearing a particular color during the funeral, having it held at a specific place, or desire for a burial/cremation should be written in it for the family to carry out.
Information on organ or tissue donation for transplant or research that requires a patient’s body to be kept on life support before their removal should also be stated in it.
Pick a health care agent (optional)
A patient may decide on whether or not to assign a health care agent. This option is beneficial because it provides flexibility for on-the-spot decision-making in the event of an occurrence of a grey area; for instance, if the agent believes that a patient’s life can be saved, they can override this form on the patient’s behalf. Hence, if a patient wishes for their preferences to be strictly adhered to, appointing a health care agent becomes redundant.
Filling the Living Will Form
The patient must state the correct information on this form as it directly impacts the medical decisions made for them if they cannot communicate on their own. The information to be filled in it includes:
An outline of treatment preferences
The patient must decide on what course of action they would like the medical personnel to take first during an emergency. They must decide on whether life-sustaining care should be provided or if they should allow natural death to take place. There are three critical treatment decisions according to categories that the patient is expected to describe in thisl form and then further specify clearly.
The three are:
- Terminal condition preferences: State a patient’s preferences in the event of an imminent death caused by injury or illness.
- Vegetative state preferences: State the patient’s preference in the event of an extended period of unresponsiveness and unconsciousness.
- End of stage condition preferences: State the patient’s preference in the event of a progressed and terminal condition where eventual deterioration leads to death.
The patient may indicate the need for palliative care even when they prohibit life-saving treatments in this document. Palliative care provides treatment for pain management and comfort until eventual death.
Establish non-medical arrangements
The writer of the will should aim to be as specific as possible when outlining their end-of-life preferences. Some of these preferences have already been mentioned in this article. However, they are not limited to the given; one can personalize as they desire.
Acquire an agent
Patients select and secure agents from their pool of family and close friends. The agent, who’s also referred to as a healthcare proxy, attorney-in-fact, or surrogate, has two main factions in this process: to carry out the patient’s wishes and make judgment calls when uncertain situations come up. Physicians or any direct health care providers to the patient cannot be agents.
An agent is also referred to as:
- An attorney-in-fact
- A health care proxy
- A surrogate
A patient must inform an individual that they are their healthcare proxy and ensure copies of the living will are provided to them along with the patient’s physician and anyone directly involved in their estate plan.
Plan how the agent can act (optional)
When a patient decides to assign medical power of attorney, it is critical that they indicate if the agent or representative is expected to follow the form till the end or, with the document’s guidance, act independently with the patient’s best interests at heart.
Obtain witness and notary signatures
When the necessary information has been filled and the patient has confirmed it with a review, the document can be executed before a notary public witness. The patient must, however, be aware that different states have different signing requirements for the living will document. Ensuring they have identified their state’s requirements will prevent any future legal turmoil.
A patient may seek qualified notary public services from local banks, libraries, or county clerks’ offices. However, the patient must know that when it comes to witnessing, specific individuals may not be allowed to act as witnesses.
They include:
- Relatives by blood or marriage
- Named individuals in the last will and testament
- Heirs to a patient’s estate
Sign the form
With the decision as to whether this document is to either be witnessed or notarized dependent on the state, a breakdown is required to help set patients on the right track.
The following is a breakdown of states and their signing requirement:
| STATE | NUMBER OF WITNESSES OR NOTARY | LAWS |
|---|---|---|
| Alabama | 2 or more Witnesses | § 22-8A-4 |
| Alaska | 2 Witnesses or Notary | § 13.52.010 |
| Arizona | 1 Witness or Notary | § 36-3282 |
| Arkansas | 2 Witness | § 20-17-202 |
| California | 2 Witnesses or Notary | § 4673 |
| Colorado | 2 Witnesses | (15-18-102) |
| Connecticut | 2 Witnesses | (Sec. 19a-575) |
| Delaware | 2 or more Witnesses | §2503. b.1.d |
| Florida | 2 Witnesses | (765.202) |
| Georgia | 2 Witnesses | (31-32-1) |
| Hawaii | 2 Witnesses or Notary | §327E-3 |
| Idaho | 2 Witness | (39-4501) |
| Illinois | 2 Witnesses | (755 ILCS 35/3(b)) |
| Indiana | 2 Witnesses | §16-36-4-1 |
| Lowa | 2 Witnesses | §144A.3 |
| Kansas | 2 or more Witnesses | (65-28,103) |
| Kentucky | 2 Witnesses or Notary | (311.625) |
| Louisiana | 2 Witnesses | (RS 40:1151.4) |
| Maine | 2 Witnesses | §5-803(2) |
| Maryland | 2 Witnesses | §5–602 |
| Massachusetts | No Statute | |
| Michigan | No Statute | |
| Minnesota | 2 Witnesses or Notary | (145B.03) |
| Mississippi | 2 Witnesses or Notary | (41-41-201) |
| Missouri | 2 Witnesses | (459.015-4) |
| Montana | 2 Witnesses | (50-9-103) |
| Nebraska | 2 Witnesses or Notary | (20-404) |
| Nevada | 2 Witnesses | (NRS 449A.439) |
| New Hampshire | 2 Witnesses | (137-H:1) |
| New Jersey | 2 Witnesses or Notary | (26:2H-53) |
| New Mexico | 2 Witnesses | (24-7A-1) |
| New York | (No Statute) | |
| North Carolina | 2 Witnesses and Notary | § 90-321 |
| North Dakota | 2 Witnesses | (23-06.5-05) |
| Ohio | 2 Witnesses or Notary | (2107.03) |
| Oklahoma | 2 Witnesses | (63 §3101.1) |
| Oregon | 2 Witnesses | (127.515) |
| Pennsylvania | 2 Witnesses | § 54-5442 |
| Rhode Island | 2 Witnesses | (§ 23-4.11-3) |
| South Carolina | 2 Witnesses | (44-77-40) |
| South Dakota | 2 Witnesses | (34-12D) |
| Tennessee | 2 Witnesses | (32-11-101) |
| Texas | 2 Witnesses | (166.032) |
| Utah | 1 Disinterested Adult | (75-2a-107) |
| Vermont | 2 Witnesses | (18 V.S.A. § 5251) |
| Virginia | 2 Witnesses | § 54.1-2983 |
| Washington | 2 Witnesses or Notary | (RCW 70.122.030) |
| West Virginia | 2 Witnesses | (§16-30-4) |
| Wisconsin | 2 Witnesses | (154.03) |
| Wyoming | 2 or more Witnesses | (35-22-101) |
Frequently Asked Questions
States provide varied differences for a living will and an advance directive. Whereas some states identify the two as functionally the same, in other states, an advanced directive contains a more extensive variety of things to a living will, such as the fact that it can include both living will and organ donation directives.
The living will document bears within it the patient’s specification on their preference of how their end-of-life care is to be handled. On the other hand, medical power of attorney gives medical decision-making powers to someone else should a patient be unable to make medical choices themselves.
An individual can write a living will without a lawyer in one day. This is because the document contains a patient’s wishes in the event of life-threatening situations.
Family members and health care providers may not know an incapacitated patient’s preferences on life-sustaining care and end-of-life care without a living will. This can cause massive strain for the family and even more agony for the already suffering patient.







