A DAP (Data, Assessment, and Plan) note is a data management tool used by healthcare providers to record, take and organize notes when tracking the progress of mental and behavioral clients
The note records the clinician’s actions and observations, the client’s answers, and professional notes during the session. Therefore, they are commonly used by therapists, psychologists, social workers, and other related professionals in medicine. It is an official document that can be shared with the client and third parties if requested based on HIPPA compliance standards.
Having an efficient and quick mental health progress notes organization tool is important in health care. This note is an example of one of the popularly used note recording and organizing tools. It is primarily focused on tracking the progress of clients. As a result, it is more oriented towards behavioral health, thus more common among therapists.
When interacting with patients, you will most likely take down an array of notes that can be used in diagnosing and treating the client. Such a note allows you to document these notes effectively without spending more time than is necessary. Once completed, it becomes part of the patient’s/client’s official file.
The data in the note is used to establish the patient’s journey and ensure there won’t be any unexplored paths at the end of the patient’s journey. Some healthcare providers sometimes include Response as a component of the DAP to create a DARP note. This article will discuss the components and other details of it to clarify further how it is used by healthcare providers, social workers, and other related professionals.
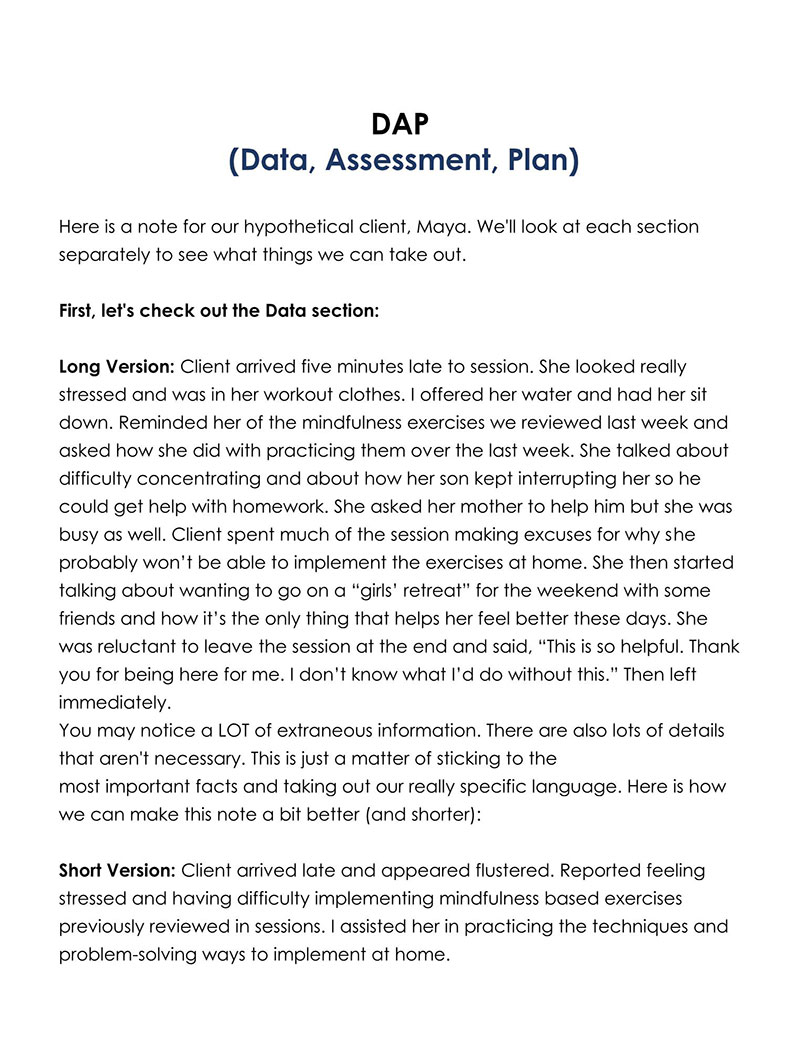
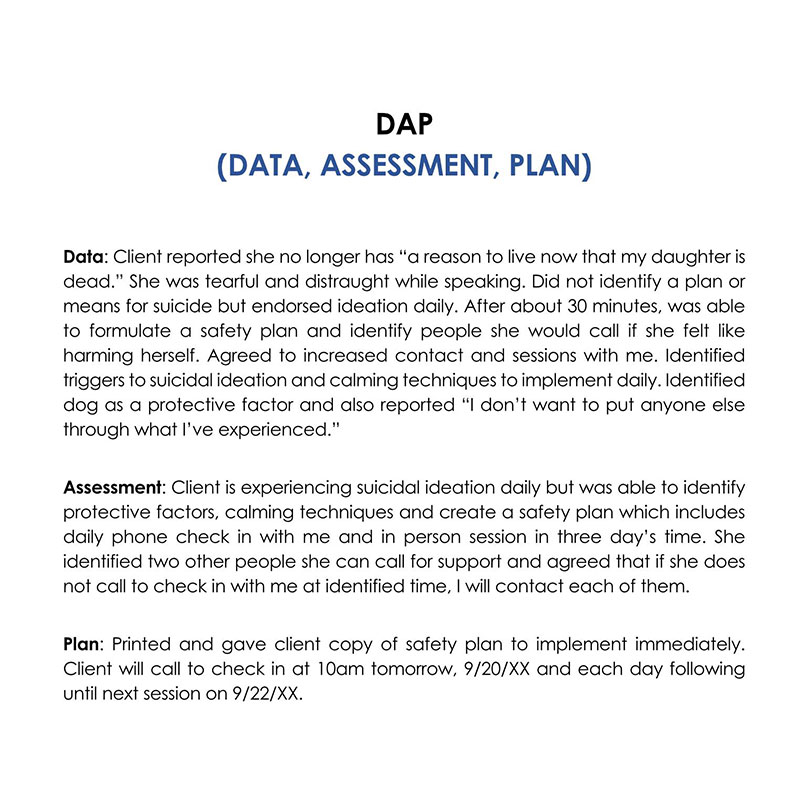
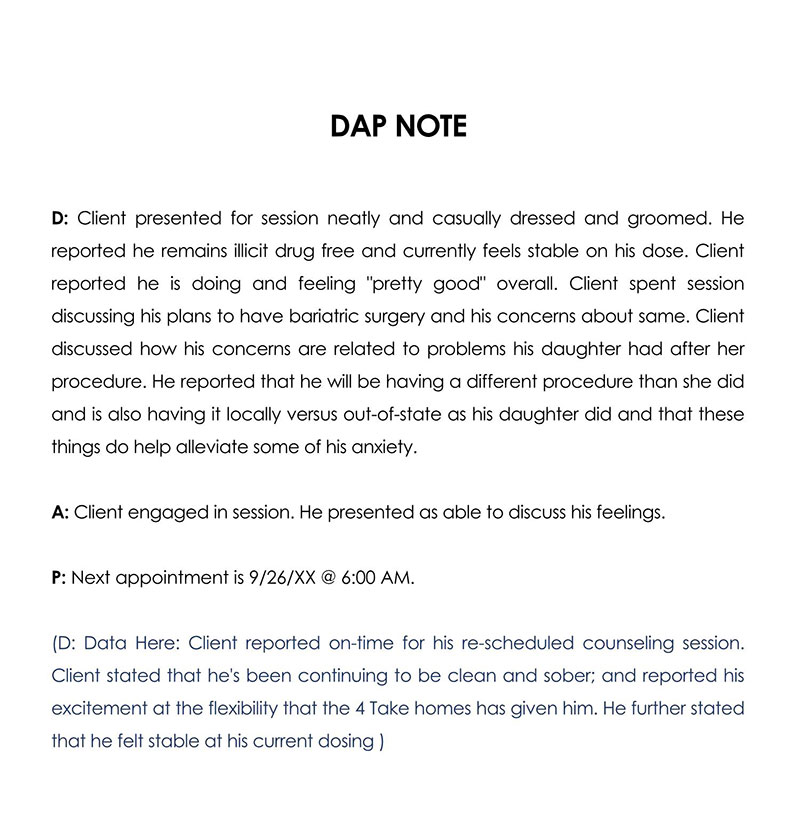
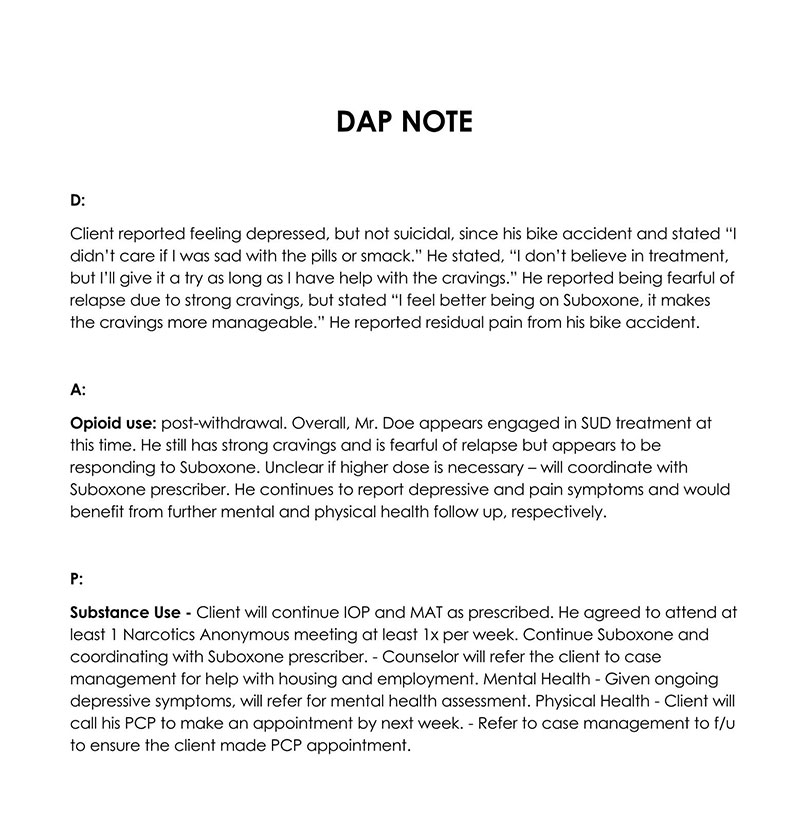
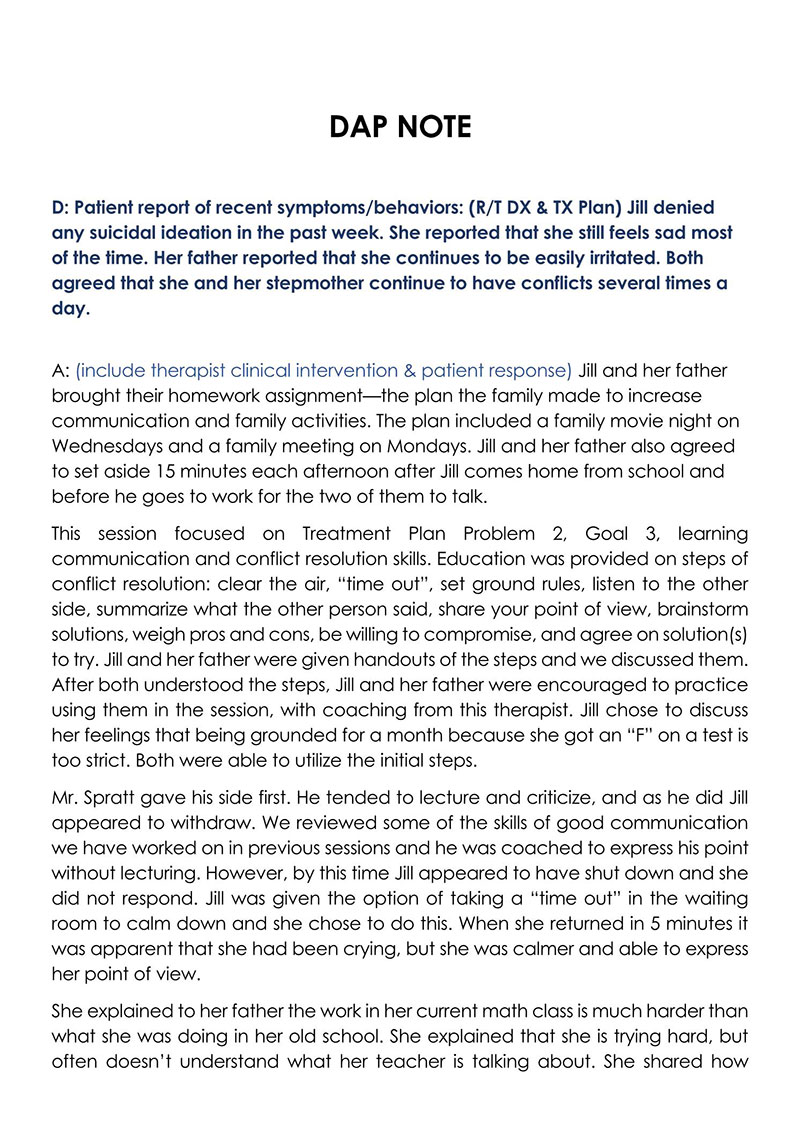
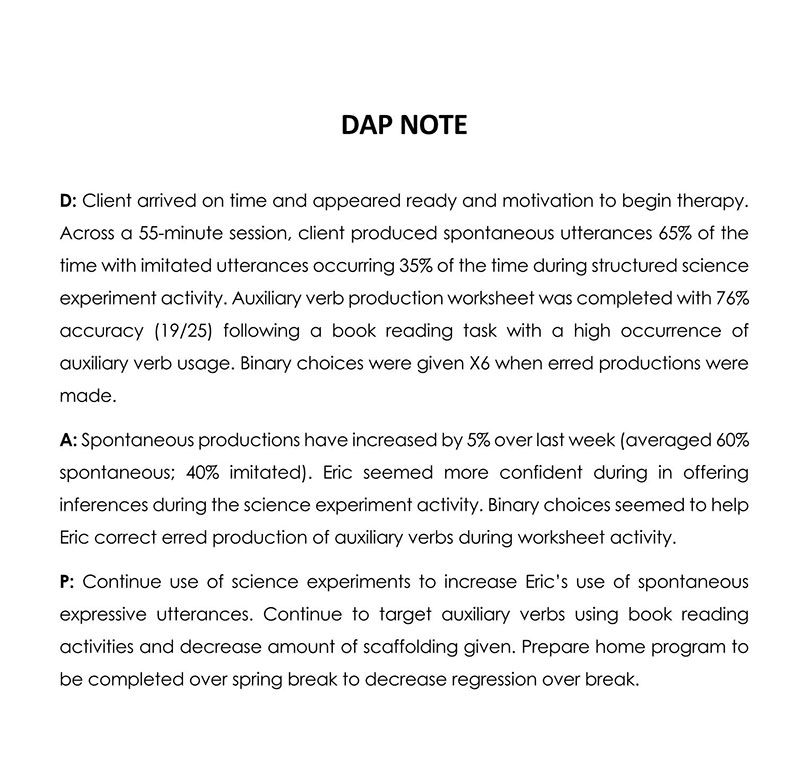
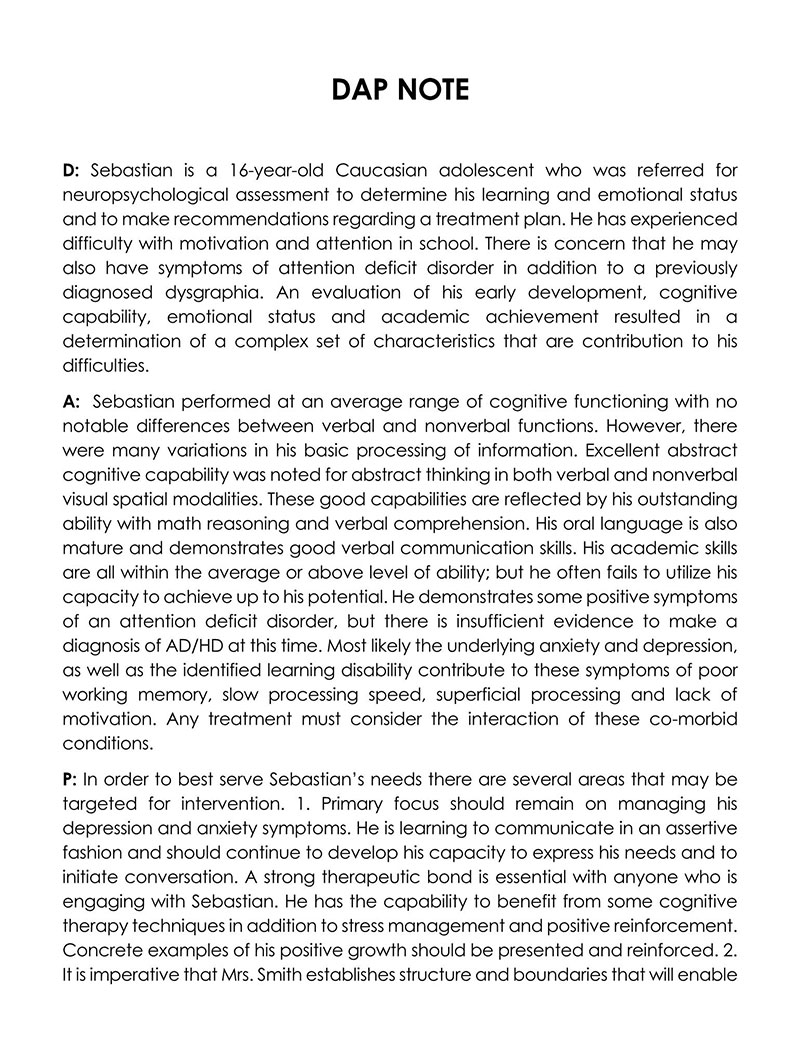
Premade DAP Notes
SOAP Vs. DAP
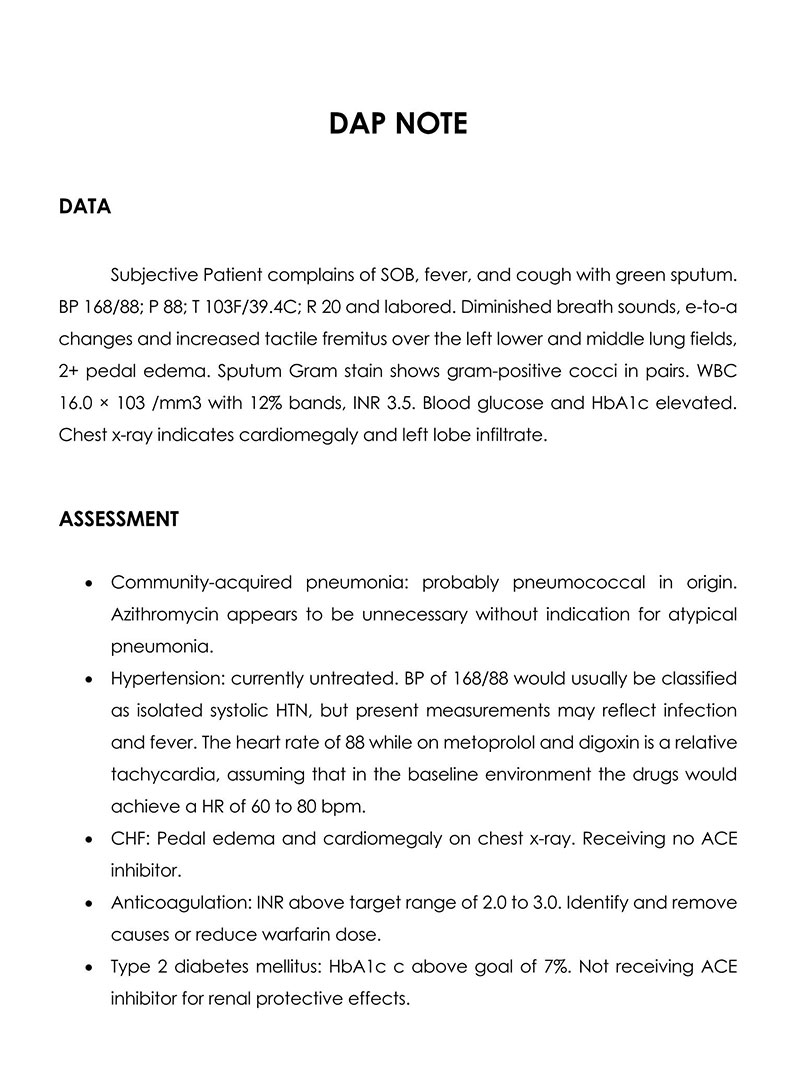
You might have heard of the term SOAP notes and wondered how they differ from DAP. SOAP (an acronym for Subjective, Objective, Assessment, and Plan) notes are equally common in healthcare. However, they should not be confused with later ones, even though they are also used to track the progress of a client’s treatment. SOAP notes have been around for a longer period than Data, Assessment, and Plan notes and are considered the industry standard for recording progress.
The major difference between the two documents is that a SOAP note splits the Data section of the DAP document into Subjective and Objective data. Consequently, this creates confusion, more so in behavioral health, when defining which data is subjective or objective. While the distinction is clear between the two in general medicine, it becomes difficult to distinguish them in psychological and behavioral healthcare using a SOAP note.
For example, when physicians record data using a SOAP note, they can collect indisputable (objective) data such as temperature or blood pressure. However, if a psychologist has to record the signs of a mental health patient, they cannot measure the degree of sadness or anxiety. Clearly, the distinction between subjective and objective data would be hard to draw.
As a result, clinicians in mental health prefer a Data, Assessment, and Plan note to a SOAP note because all the data can be categorized under Data without struggling to define what is subjective or objective.
Regardless of the difference between the two documents, any data collected is used to assess and create a treatment plan for the client.
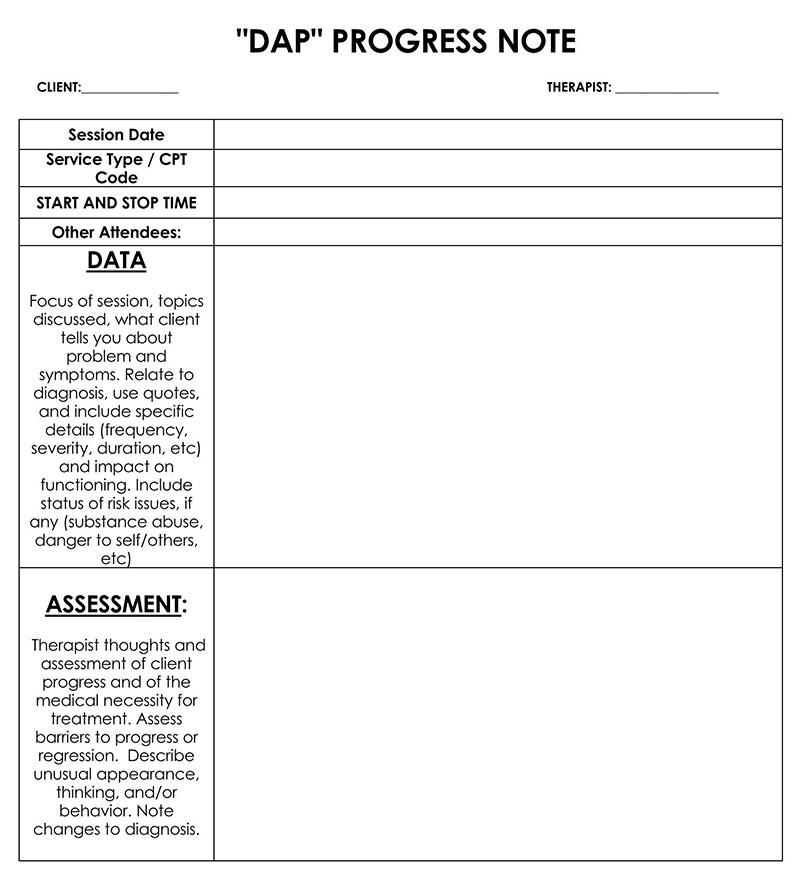
Essential Components of a DAP Note
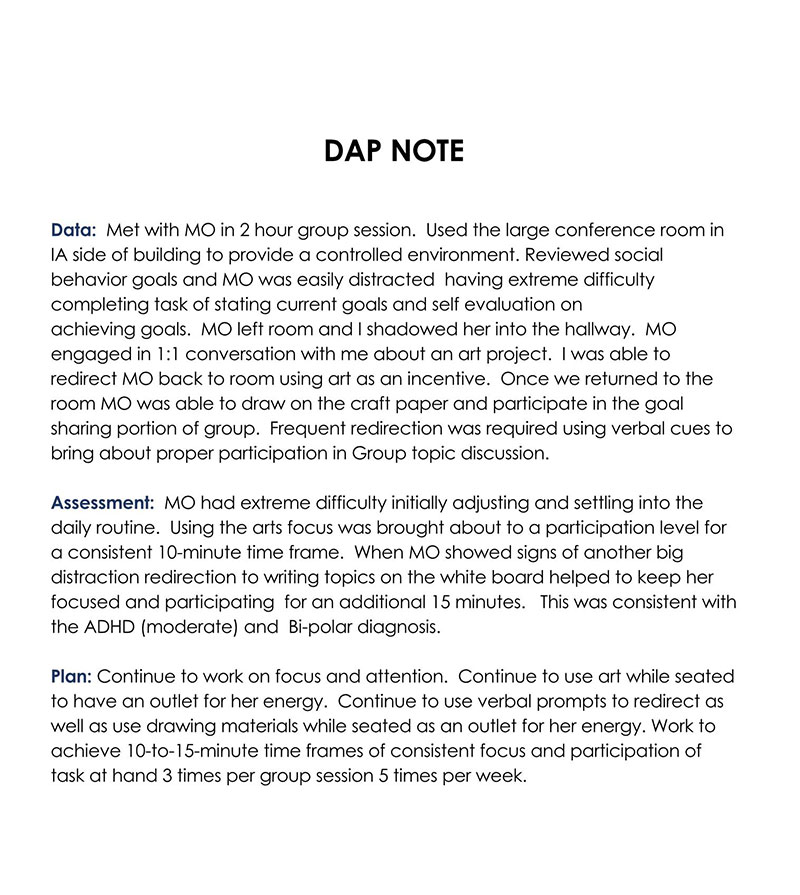
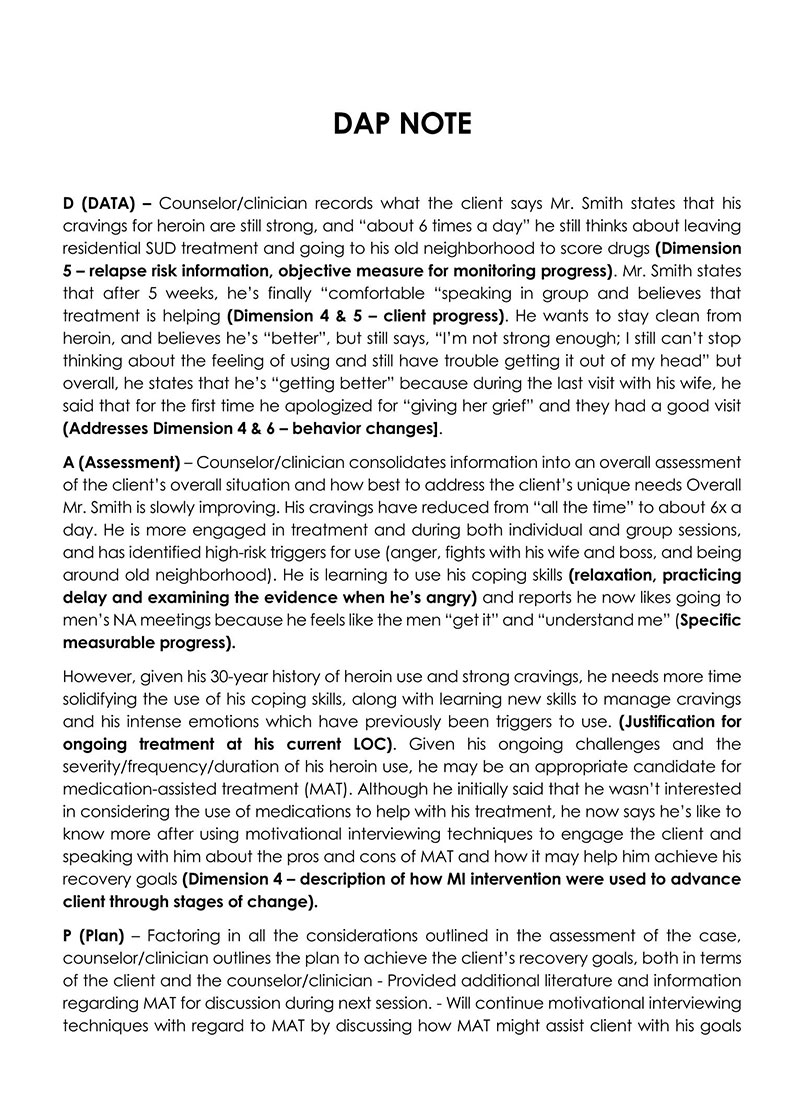
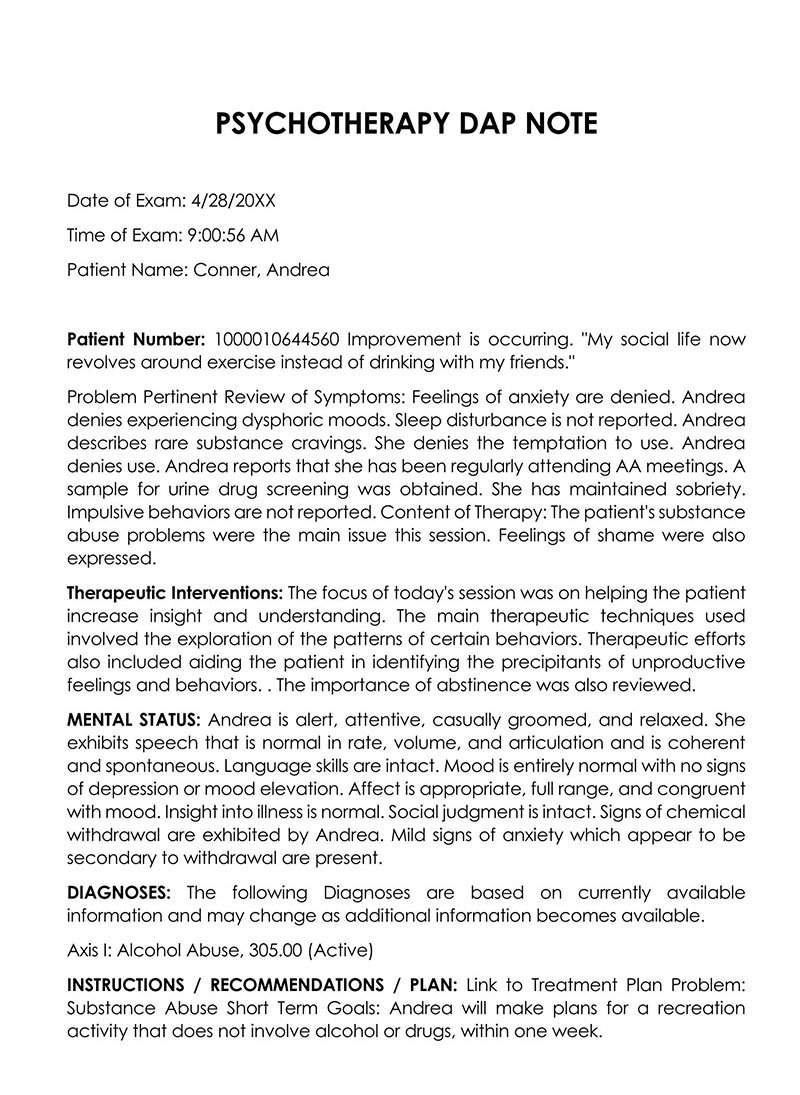
It should have three basic sections; Data, Assessment, and Plan. It can also have a Response section depending on the circumstances or nature of the session with the client. The information in each section should be based on direct interactions and observations with the patient.
Each section differs, as discussed below:
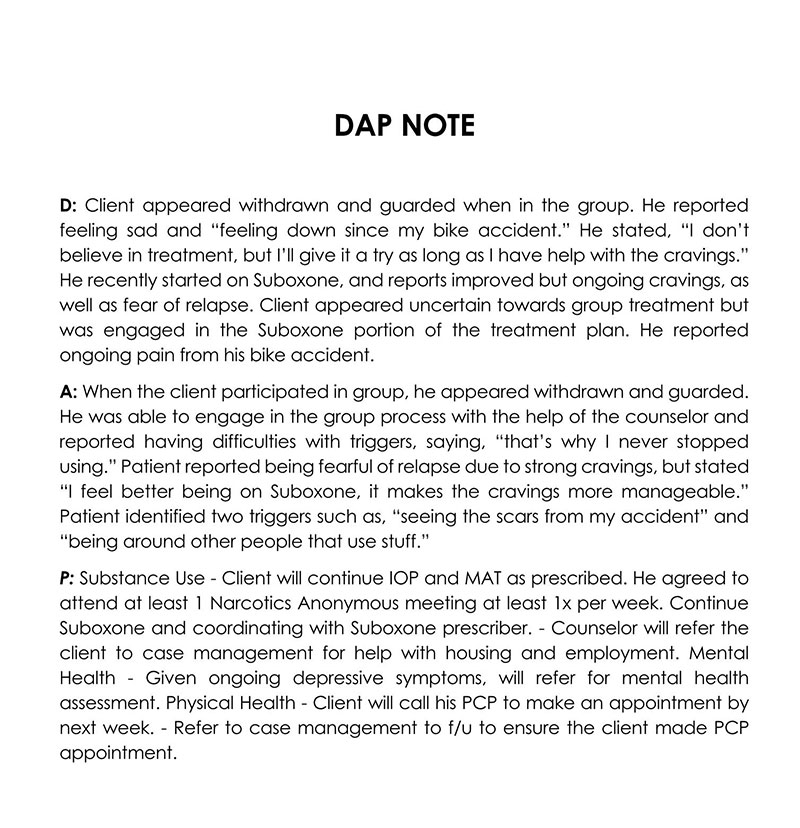
Data
The data section should capture all significant observations made during the session. In addition, you are expected to write down any notes you want to base your recommendations. Information in this section includes behaviors, signs, reactions, answers, etc., that relate to the probable condition or illness in question.
Assessment
Any information collected during the session must be interpreted to provide direction toward the appropriate treatment options. Basically, this section of the note answers, “what does the data recorded mean?” In this section, you are required to utilize your professional know-how. It marks the transition from data to partial professional subjectivity. This will often involve comparing, contrasting, and analyzing the client’s overall physical and behavioral traits.
Plan
The plan of action is the last section of it. The plan should include precise and objective actions and interpretations to help the client. You can also follow the recommended steps and agenda of the subsequent session. Alternatively, if the client is already undertaking a treatment plan, you can recommend whether the plan should be continued, foregone, or modified based on the assessments made in the assessment section.
The plan can be accompanied by a schedule, for example, documenting the time intervals between the current appointment and the next. The DAP is a progress note-taking tool; therefore, it doesn’t record the patient’s entire treatment plan but treatment goals from one session to the next.
Response
If you want to include the response section in this note, you can do so. However, note that it should be added as an extension of the assessment section. This section records the patient’s response to your professional assessment. Patients react differently to assessments. Some might get aggressive, angry, defensive, mute, etc.
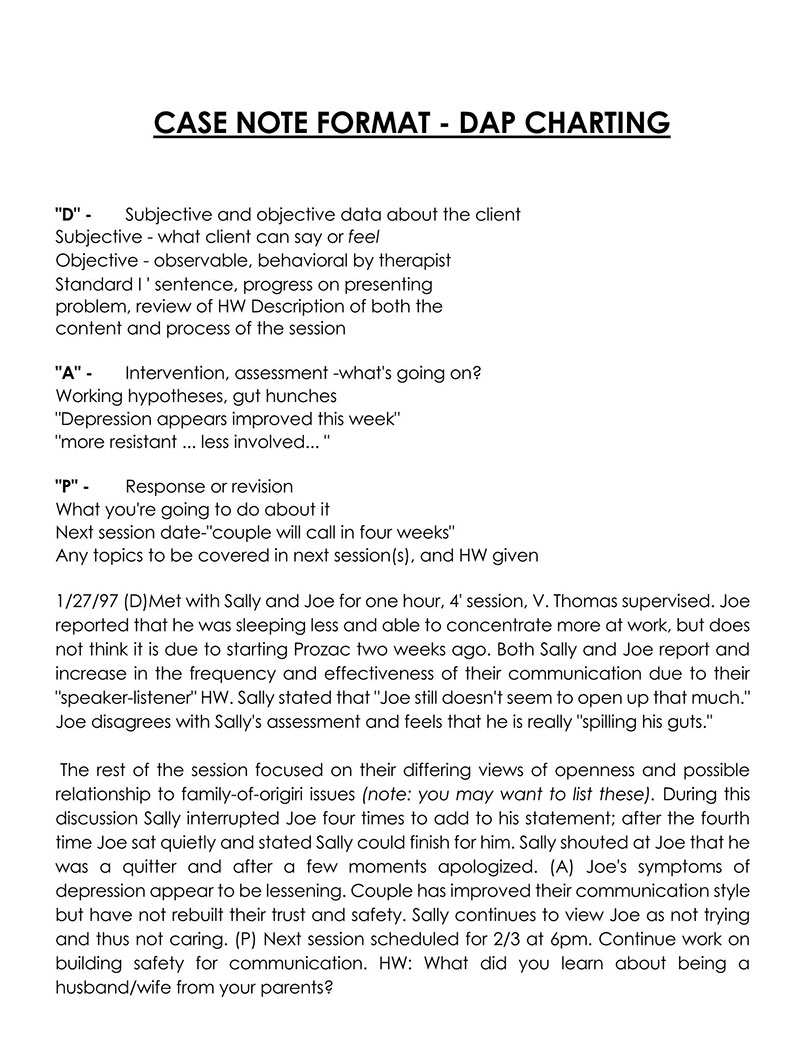
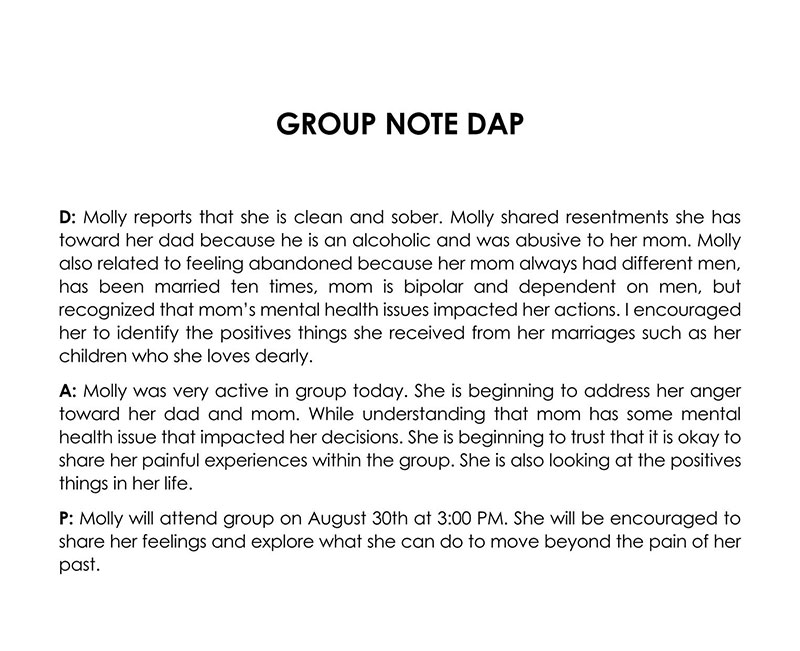
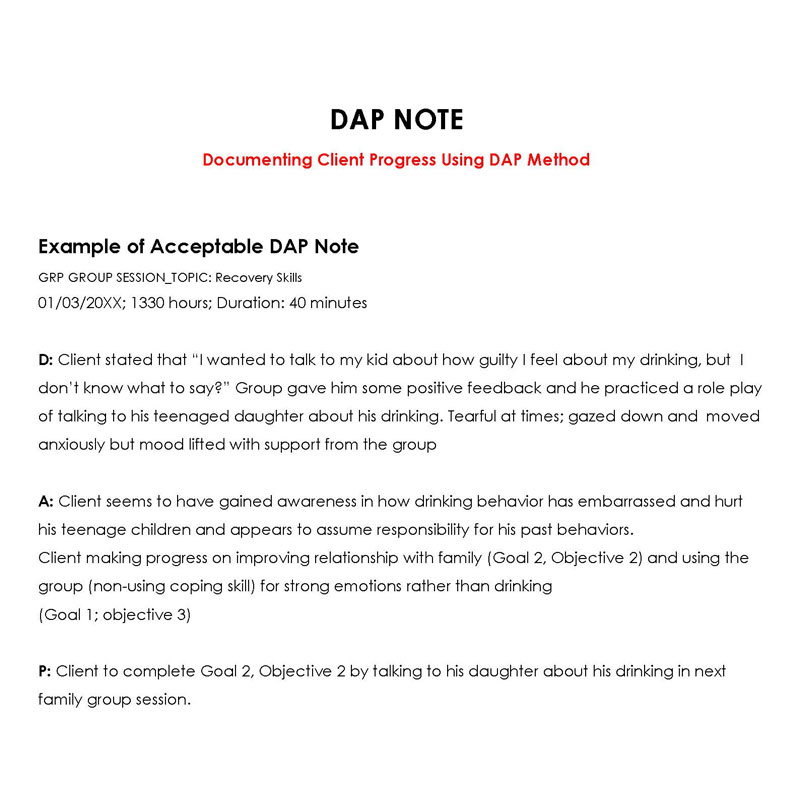
DAP Notes Example
Patients name: Jared Meyers
Data
The patient appeared exhausted. He had bloodshot eyes. He spoke faster than usual and had a high pitch in his voice. He kept looking at the door. He claimed to be doing better than in the previous session. He claimed his family does not understand him and does not want to continue with school. He claimed his parents are on the verge of a divorce. He exhibited signs of paranoia whenever there were sudden movements in the room.
Assessment
The patient has not been having enough sleep. This might be due to stress. There were signs of abuse of stimulants. Therefore, amnesia could be a possibility. Family issues and trauma might be the driving factor behind his paranoia. Lack of support at home could be the primary cause of his reduced motivation in school.
Plan
A medical examination and drug tests. Recommend a family therapy session. The medical and lab report is to be reviewed in the next session.
Do’s and Don’ts
The more well-written this note is, the more effective it is in treating the patient. You can incorporate the following do’s and don’ts in it:
Do’s to keep in mind
The following considerations can help you improve the quality of such a note:
Define your perfect note
Before beginning your note, you should understand what a perfect note will comprise. This means you must be aware of what you want to achieve with the documents so you can define the document’s specific requirements.
You should know which information you will be looking forward to collecting from the session. You can declare that your data section will be recorded as bullet points while the assessment section will be written as comprehensive sentences.
Know your audience
You should consider the readers before and when writing the document. Since it may be shared with other professionals at some point in the future, it should be written in a professional tone. Remember that the note will go in the client’s file as an official record of the session and thus should be formatted and organized as a formal document.
Utilize documentation tools
Using the best-suited tools can simplify the process of taking notes using this note. You can focus on the efficiency and sharing elements of the document. Using online templates for it can prove beneficial as it is easy to update and fast to share with third parties. You can also consider whether you prefer typing or handwritten notes; you should use tools that assist you in whichever method you prefer.
Don’ts to avoid
You should avoid the following things to ensure the note serves its purpose effectively:
Don’t write too much or too little
Always focus on inputting the proper and necessary details only. You should put enough information to be used as a foundation for assessment and little enough to make the note easy to understand.
Don’t make it complex
It should be direct to the point. Remember, the document is not a personal record of the session but an official record. Therefore, other people will interact with it at one point or another. You need to write it in a way that other people can comprehend how the information recorded is important to the patient’s health. Having well-defined objectives at the beginning of the sessions is one way of ensuring you capture valuable information.
Avoid using tools that don’t work for you
You are not obligated to use sophisticated tools when writing it. Use tools that increase the efficiency of the process and produce a quality document. If you prefer working slowly, you can opt to use handwritten notes instead of a template. However, if you have illegible handwriting, consider typing the document.
Final Thoughts
Data, Assessment, and Plan notes are recommended for healthcare providers such as therapists who frequently attend to the same patients. It is used to record pertinent details determined during each session. Notes recorded in the document should not be confused with personal evaluation notes. A DAP is an official record of the patient’s treatment. The document can be typed or handwritten. However, it must be clear and easy to interpret should third parties require the document.