Nursing notes are written records that nurses maintain to document important information about the care and treatment provided to patients.
These notes serve as a communication tool among healthcare professionals and provide a comprehensive record of the patient’s condition, interventions, and responses to treatment. The notes are typically brief, objective, and focused on essential details related to the patient’s health status, nursing assessments, interventions, and outcomes. They may include information such as vital signs, medication administration, wound care, patient observations, changes in condition, patient education, and any other relevant details that contribute to the patient’s overall care plan. They play a crucial role in promoting continuity of care, facilitating effective communication, and ensuring accurate documentation for legal and regulatory purposes.
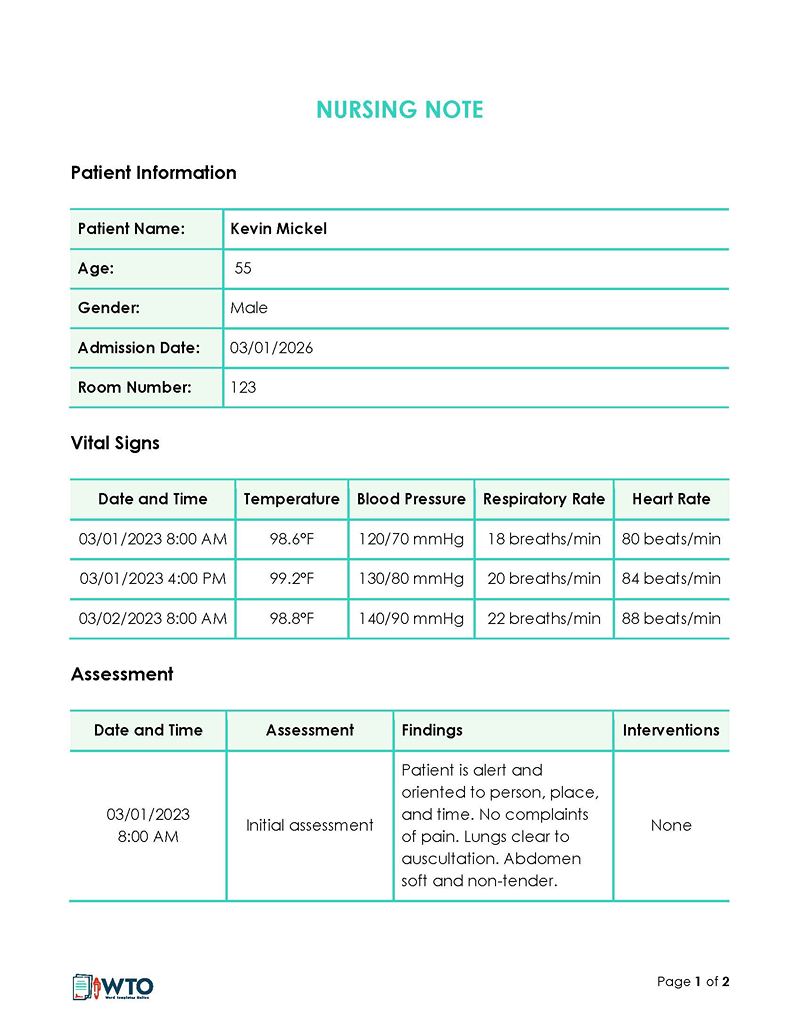
EXAMPLE 1
The patient has made positive progress since being introduced to the new medication. No shivering or pale eyes. A high fever was noted. May need further tests as he reports frequent headaches.
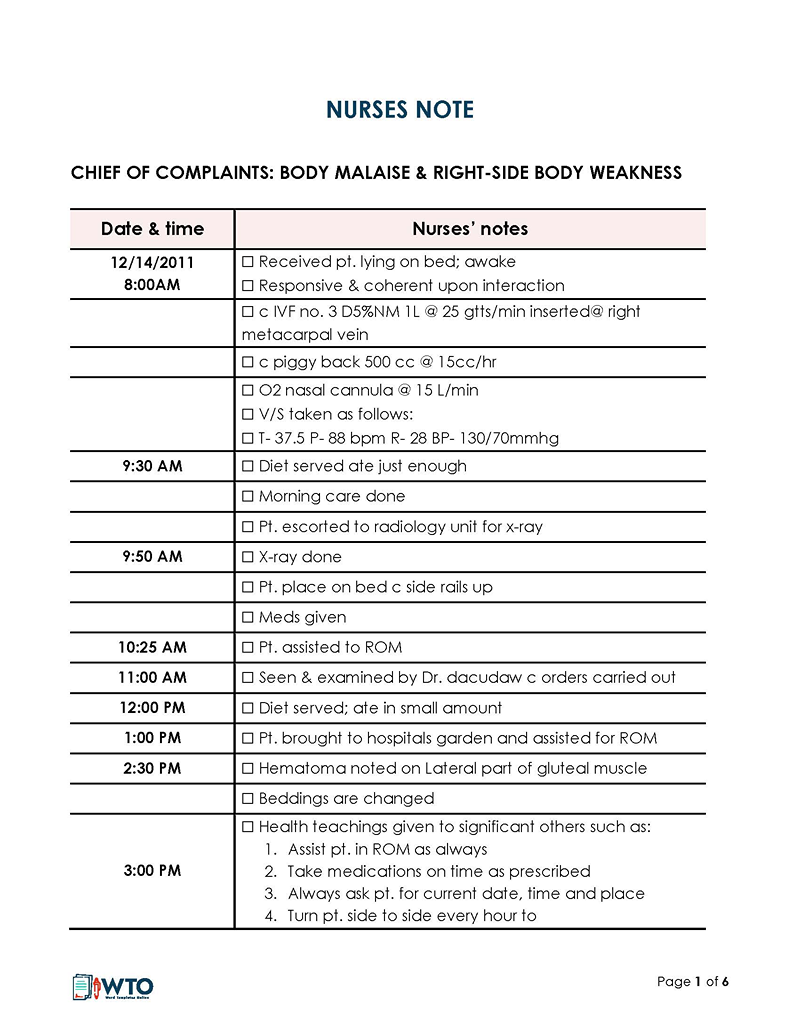
EXAMPLE 2
During the 4 p.m. routine check-up, the patient’s BPM had risen to 84 B/S. High temperatures were recorded. The patient reported acute pain in the chest and numbness in the left limbs.
This article discusses the importance of nursing notes. It also guides nurses on what information to include in a comprehensive and useful note. Lastly, it provides several examples to highlight the pros and cons of different types of these notes and help you better understand how to write such documents.
Reasons for Using Nursing Notes
The notes serve as a crucial documentation tool for healthcare professionals to accurately record and maintain essential information about the patient’s condition, assessments, interventions, and outcomes. They provide a detailed account of the care and treatment provided to the patient during their stay in a healthcare facility.
The reasons for maintaining these notes include:
Legal record
The note is a legal record of any interventions to address a patient’s medical condition. It is admissible evidence of ethics, competency, and proof that standard medical care was provided to a patient. They are considered a legal record of the patient’s condition, the interventions performed, and any responses or outcomes observed. Accurate and detailed notes are crucial for legal and regulatory purposes, such as medical audits, insurance claims, and litigation.
Communication
This document helps facilitate effective communication among all healthcare providers interacting with patients. They provide a means of sharing critical information, such as changes in the patient’s condition, treatment plans, and important observations. This ensures that all team members are well-informed and can provide consistent care.
Planning and coordination
They provide a reference for ongoing care planning. They outline the patient’s current condition, nursing diagnoses, goals, and the proposed interventions. The document helps healthcare professionals develop individualized care plans and track the progress or effectiveness of interventions.
Monitoring
They facilitate the evaluation and monitoring of a patient’s condition and response to interventions. By documenting observations, vital signs, symptoms, and patient responses, nurses can track trends, identify patterns, and assess the effectiveness of treatments or interventions over time.
Care planning
Documentation is vital to providing efficient medical services. The notes provide a reference for ongoing care planning. They outline the patient’s current condition, nursing diagnoses, goals, and proposed interventions. The notes help healthcare professionals develop individualized care plans and track the progress or effectiveness of interventions.
Research and education
They contribute to research and education in healthcare. The data recorded in the notes can be used for evidence-based research meant to improve medical care. Anonymous and de-identified data from the notes can be analyzed to identify trends, outcomes, and best practices. They also serve as educational resources for students, allowing them to learn from real-life patient scenarios.
Billing purposes
They play a significant role in billing and reimbursement processes, as they serve as a comprehensive record of the services rendered to the patient. By accurately documenting the care provided, the notes ensure that healthcare providers can effectively substantiate their actions and facilitate appropriate billing and reimbursement procedures.
Nursing Note Vs. Charting
Nursing notes and charting are both forms of documentation used in healthcare settings, but they serve slightly different purposes.
The notes are summaries of a patient’s health, assessments, and a nurse’s key decisions made at a particular time, whether it is during a nursing visit or routine check-up. Charting refers to the broader documentation of a patient’s medical information in their medical chart or electronic health record (EHR). It is the compilation of all documentation required from nurses, including professional, legal, and internal documentation.
Additionally, only objective information is used in charting.
EXAMPLE
Examples of such information include test results, IV site documentation, alarms, patient demographic documentation, etc., which are set up according to the specific protocols of the medical facility. Notes are examples of chart documents.
The key difference between nursing notes and charting lies in their focus and level of detail. The notes primarily capture nursing-specific care and interventions, while charting encompasses a broader scope of medical information from various healthcare providers. The notes provide a more in-depth account of the nursing care delivered and the patient’s response, while charting presents a comprehensive overview of the patient’s medical condition and treatment across disciplines.
It is important for healthcare professionals to maintain accurate and timely documentation in both nursing notes and charting to ensure effective communication, continuity of care, and legal compliance. The specific documentation requirements may vary depending on the healthcare setting, organization policies, and regulatory guidelines.
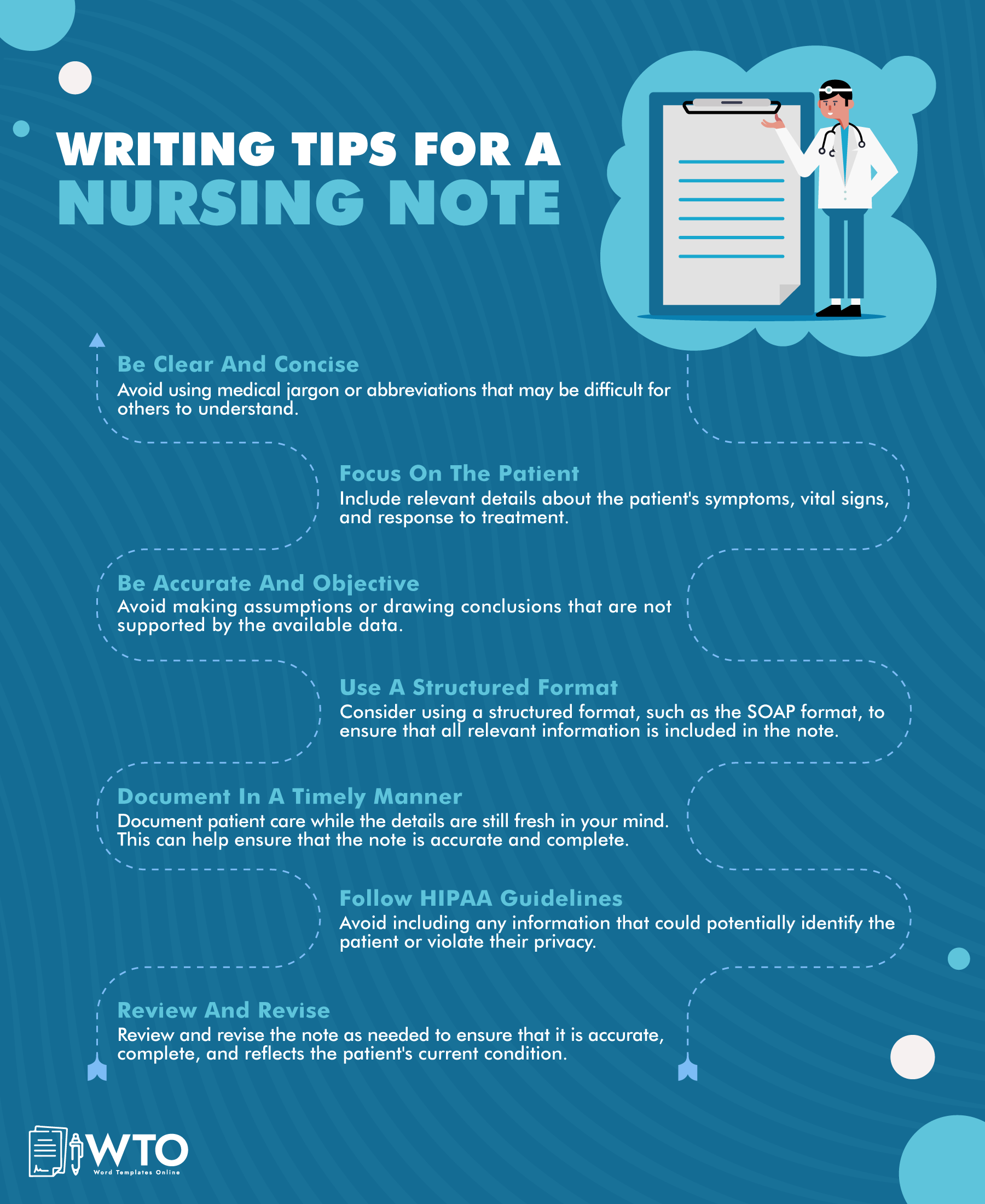
What to Include in a Nursing Note
Documentation can greatly impact nursing care plans and physicians’ decisions. Therefore, it is critical to ensure accurate, clear, and informative notes are written so medical practitioners can see the interventions and progress made over time.
You must outline the following specific information in an informative note:
Date and time
Time stamps provide an accurate and chronological record of events, actions, and observations. They allow healthcare professionals to track the sequence of patient care activities, which is crucial for maintaining an accurate medical history and ensuring continuity of care.
Besides that, they are important for legal and documentation requirements. They provide a clear timeline of events and actions taken, which can be essential in legal proceedings, audits, or investigations. Accurate and timely documentation is critical for demonstrating the standard of care provided and ensuring compliance with regulatory standards. Therefore, you must indicate the date and time on the document.
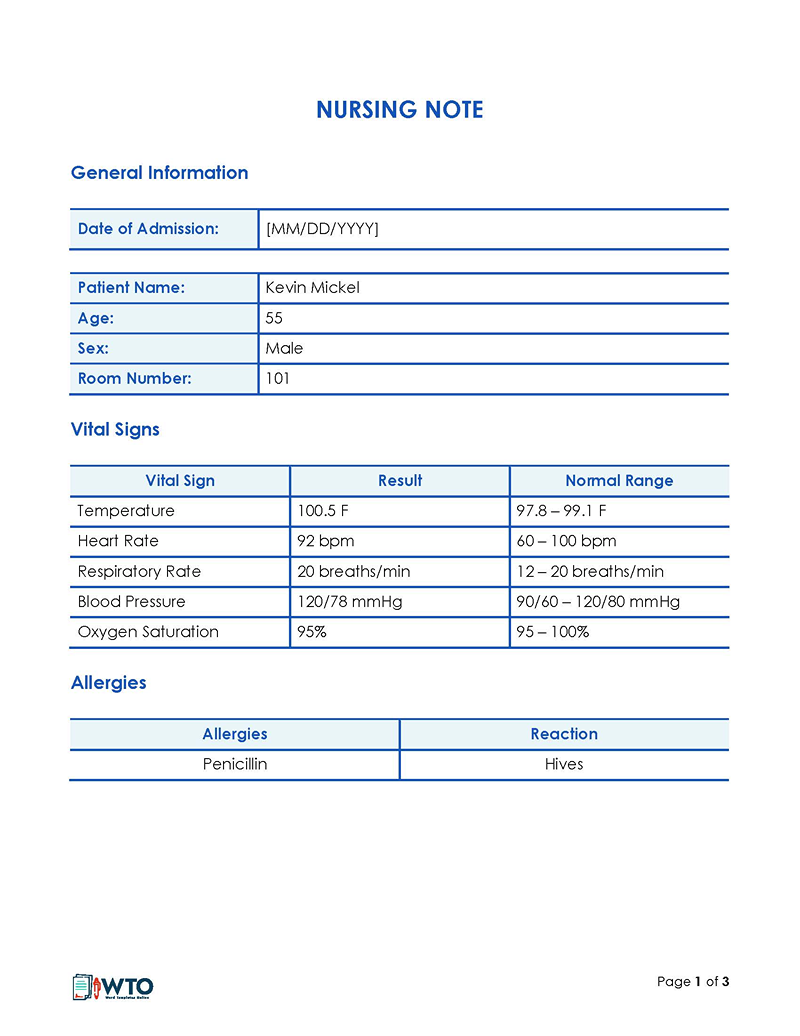
Patient’s details
The document must specify the patient being referenced.
EXAMPLE
This requires you to include information such as the patient’s name, age, and gender. Identifying information, mitigating the potential for file confusion, and streamlining the organization and archiving of records.
Furthermore, the inclusion of specific identification details greatly facilitates future referencing and retrieval processes.
Name of the nurse
Including the name of the nurse on the notes is vital for accountability, effective communication, and meeting legal and documentation requirements. It ensures that the responsible healthcare professional can be identified and contacted regarding the documented information. Additionally, it supports seamless collaboration among healthcare providers and facilitates continuity of care for the patient. The name on the document also aids in quality improvement initiatives and adherence to established standards.
Reason for visit
An informative note will include what the patient reported as the purpose of their visit. This entry records their chief complaint. This information is typically subjective, and the patient will state how they feel. This often refers to normal body functioning or performance changes.
EXAMPLE
Most patients will state their level of pain, thoughts, concerns, and symptoms, such as fever, headache, rash, nausea, etc.
Appearance
You must document any physical observations about the patient. This information is objective and strictly based on what can be seen.
EXAMPLE
A patient may appear fatigued, swollen, itchy, immobile, etc., which must be recorded in the note.
Vital signs
Vital signs include measurements such as blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation. These measurements provide valuable information about a patient’s physiological status and help healthcare professionals monitor their overall health and response to treatment. In the notes, documenting vital signs allows for tracking changes over time, assessing trends, and providing a comprehensive record of a patient’s condition. It assists in evaluating the effectiveness of interventions and contributes to the overall assessment and care planning process.
Observations and findings
Notable observations made during the shift, such as changes in the patient’s physical appearance, behavior, mental status, or any relevant findings from assessments or examinations.
Labs and diagnostics
You should also document any lab tests and diagnostic procedures that are required after the assessment. They are ordered to determine the specific disease or condition affecting the patient. A treatment plan is then formulated based on the findings. Examples of such tests and procedures include blood analysis, gastric fluid analysis, TSH test, etc.
Changes or updates
Any changes in the patient’s condition, response to treatment, or notable events that occurred during the shift. This may include critical incidents, improvements, deteriorations, or any concerns that need to be communicated to the next shift or the healthcare provider.
Instructions
It is important to record any instructions directed to the patient regarding medications or lifestyle changes to improve their condition further. This section will let you include technical details such as increased dosage and revised treatment plans. Notable safety concerns or precautions that need to be communicated, such as fall risks, infection control measures, or specific patient needs must also be stated.
Family interactions
An informative note will also document any interactions you have had with the patient’s family members. Relatives are sources of helpful information that can be used to develop treatment plans.
Recommendations and observations
Any recommendations that you or the doctor have made can also be stated. These may be in regard to additional tests or visits to specialists. This information can help direct all the health personnel that need to be engaged to treat the patient.
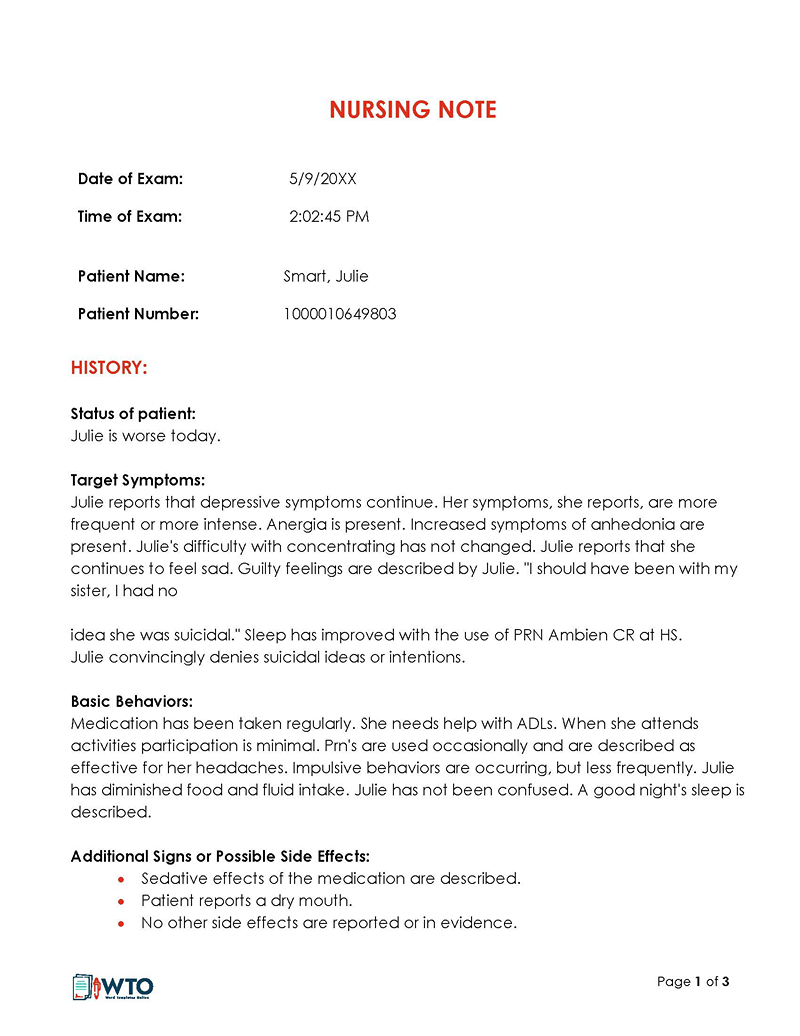
Unusual findings
If there are any unexpected or atypical observations or findings during the shift that may require further investigation or attention, they can be mentioned in the report. For example, if a patient suddenly develops a new symptom or if there is an unexpected response to treatment. Similarly, if there are any significant emotional or psychosocial factors impacting the patient’s care or well-being, such as notable emotional distress, family dynamics, or cultural considerations, these can be mentioned to provide a more holistic understanding of the patient’s situation.
Note about what not to include: Information that should be avoided includes opinions and speculations regarding the patient’s feelings. Also, the note must not record personal information from family members or friends. Confidential conversations must also not be documented. It is unprofessional to write negative comments about other staff members. The nursing report should maintain a professional and respectful tone. Inappropriate language, offensive remarks, or derogatory comments should never be included. Lastly, you should not include any information listed in the Institute for Safe Medication Practices’ (ISMP) list of abbreviations.
Free Templates
Nursing Notes Examples
There are different types of nursing notes in healthcare. Each type has its advantages and disadvantages. Below is a discussion of how three common types of notes differ.
Also, the examples can provide insights into the proper structure of the document:
Narrative nurse note
A narrative note has a story-like approach. In several paragraphs, it describes the patient’s condition, interventions, and response to treatment. It provides a more detailed account of the patient’s condition, which makes it more suited for ambiguous and complicated medical cases where detailed information is needed to diagnose and formulate treatment plans.
EXAMPLE
On 10/03/2023, 16:00, Josh Hinds reported to the front desk complaining about severe pain in his right hand and abdomen. He was sweating, claimed to be dizzy, and had fainted earlier in the day. He reported mild abdominal pain that had existed for a month but worsened approximately 2 hours ago. Josh ranked the pain at 8/10. Josh was admitted to ward C, bed 105. He was administered painkillers at 16:10. BP 100/75, P 75 T 100.8. Sweating, shivering, having bloodshot eyes, and flinching upon touching the area of concern.
Carrie Shelton. RN
Benefits and limitations
Narrative notes are advantageous as they are detailed, allowing you to collect details regarding the patient’s health status. Also, they are easily combined with other documentation. Additionally, you can adopt your own style for writing narrative notes, making the documenting process more flexible.
Additionally, the lack of standardization in format and style across narrative notes can make it challenging for other healthcare providers to quickly locate specific information, leading to inefficiencies. Moreover, narrative notes may contain subjective interpretations of the nurse’s observations and assessments, making it difficult for other healthcare providers to objectively interpret the documented information.
Furthermore, narrative notes often include excessive information that may not be relevant to the current patient’s condition or care, resulting in information overload. Repetitive documentation across multiple notes can also be a problem, making it harder to identify new or updated information efficiently. From a legal and liability perspective, they can be easily misinterpreted or contain ambiguous documentation, potentially impacting patient safety and legal defense in cases of dispute.
Progressive nursing note
These notes are recorded during a patient’s hospital stay and document details of the regular check-ups with the patient. Such notes record the patient’s care to ensure an up-to-date record of their recovery progress. The notes can be referenced when formulating new treatment plans to address any changes in the patient’s health status.
For example, a progressive nursing note will be written as follows:
EXAMPLE
Date: 10/03/2023
Time: 14:00
Patient name: Amy Kindle
Gender: Female
Medical Record Number: [Medical Record Number]
Nurse on duty: Mary Higgins
The patient reports experiencing mild to moderate abdominal pain since yesterday evening. The pain is localized in the lower right quadrant, and she rates it 5 out of 10 on the pain scale. The patient states that the pain is continuous and worsens with movement. No associated symptoms such as nausea, vomiting, or changes in bowel movements were reported. The patient states that they had a normal bowel movement this morning.
Vital Signs
Blood Pressure: 120/80 mmHg
Heart Rate: 78 beats per minute
Respiratory Rate: 16 breaths per minute
Temperature: 98.6 degrees Fahrenheit
Benefits and limitations
Such a note is advantageous as it gives a comprehensive overview of a patient’s progress, making it useful for communication and collaboration purposes. Progressive notes allow for a comprehensive overview of the patient’s condition and treatment progress over time. It helps healthcare providers to understand the patient’s medical history, ongoing care plans, and response to interventions, facilitating better continuity of care. This format also enables real-time documentation of changes in the patient’s condition, ensuring that important information is captured promptly. This allows healthcare providers to monitor trends, respond quickly to deteriorations, and make timely adjustments to the treatment plan.
The downsides of this format are that it is time-consuming for nurses to record notes during other tasks. Also, the notes may require repetitive information, which can be tedious and frustrating to write. If not well-organized or structured, progressive notes can become disorganized and difficult to follow. It may be challenging for other healthcare providers to understand the sequence of events or the most recent status of the patient.
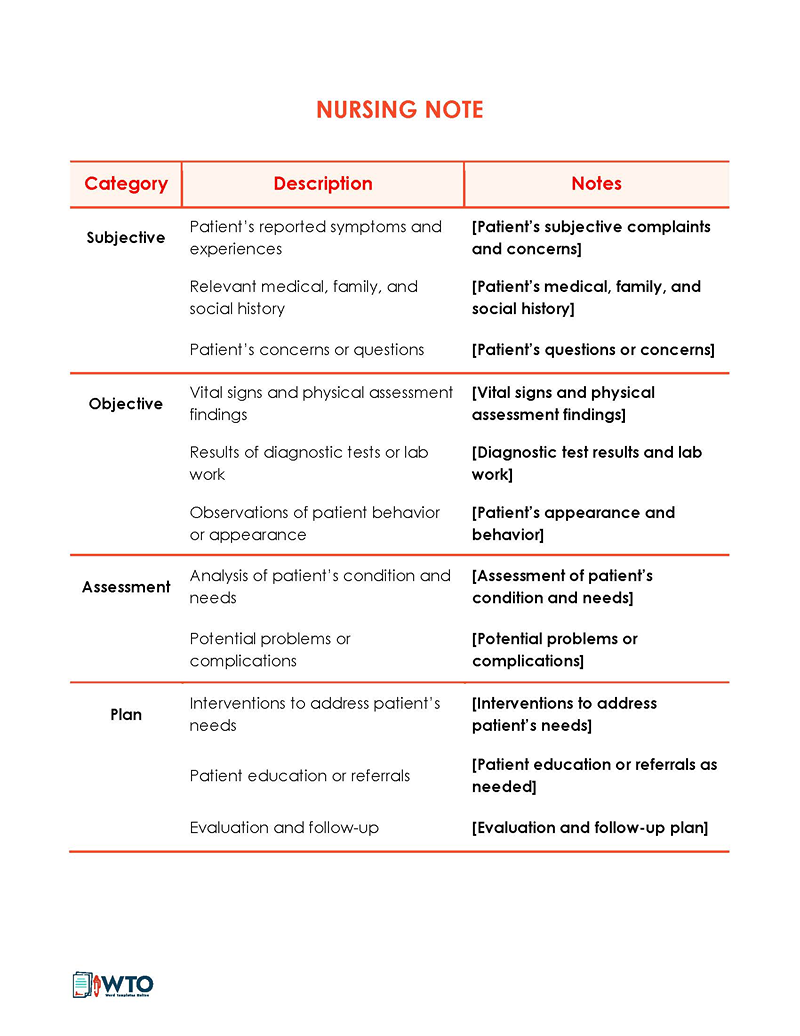
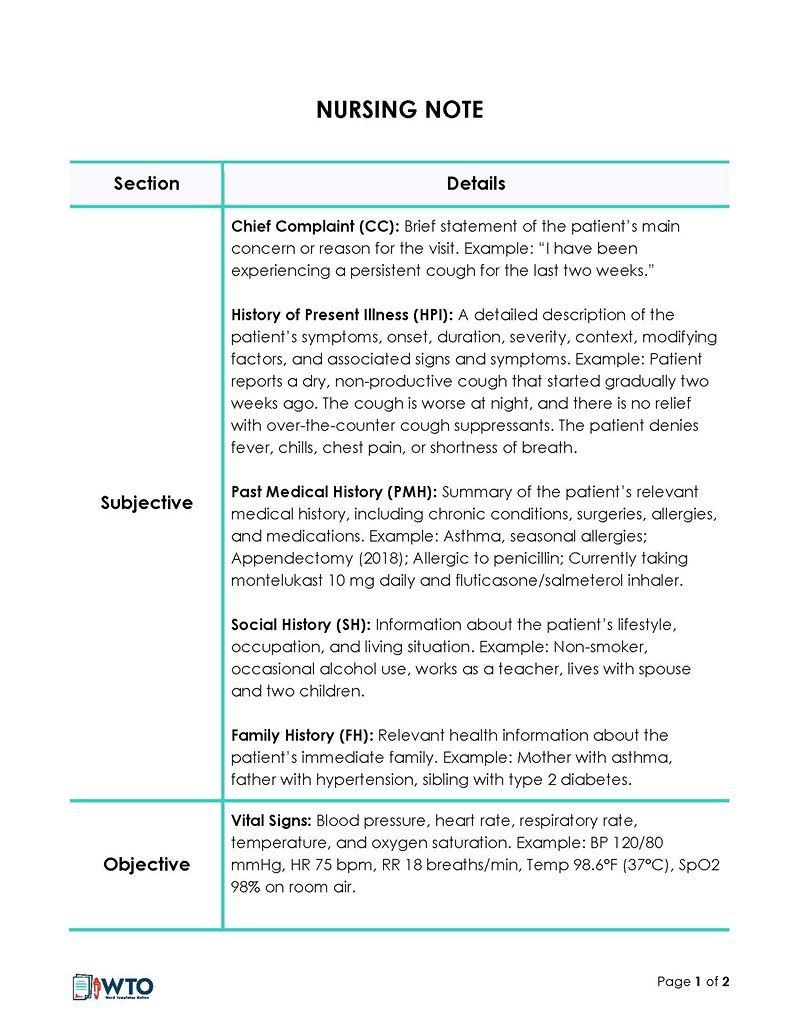
SOAP nursing note
This type of note follows the SOAP method of documentation, which involves recording nursing care notes under the following categories – Subjective, Objective, Assessment, and Plan. The subjective section documents the patient’s symptoms and history. The objective details include medical findings, and the assessment captures the diagnosis. The last category documents the proposed treatment plan and future procedures or tests. This type of structuring ensures consistency in notes from different practitioners.
A good example of the structure of a SOAP nursing note is as follows:
EXAMPLE
Name: John Doe
Date: March 10, 2023
Time: 11:00 AM
Nurse: Zoey Smith
Subjective
–John complained of frequent headaches during the night
–He reported a lack of sleep in the last 2 weeks
–He states that he is always fatigued
Objective
Vital Signs:
–Blood Pressure: 120/80 mmHg
–Heart Rate: 88 bpm
–Respiratory Rate: 20 breaths per minute
–Temperature: 98.6°F
–General Appearance: Patient appears fatigued, with slightly labored breathing. No acute distress observed.
–Lungs
Diminished breath sounds at the bases. Coarse crackles were heard bilaterally on auscultation.
–Chest X-ray
Findings consistent with bilateral lower lobe pneumonia.
Assessment
Based on the subjective and objective data, the patient is diagnosed with bilateral lower lobe pneumonia.
Plan
–The administrator prescribed antibiotics (Amoxicillin 500 mg, 3 times daily) for 10 days to treat the infection.
–Provide supplemental oxygen therapy as needed to maintain oxygen saturation above 92%.
–Encourage increased fluid intake to promote hydration and thinning of respiratory secretions.
–Administer over-the-counter cough suppressant as needed for symptomatic relief.
–Educate the patient about the importance of completing the full course of antibiotics and respiratory hygiene measures (covering mouth when coughing, hand hygiene, etc.).
–Schedule a follow-up appointment in one week to reassess the patient’s progress and adjust the treatment plan if necessary.
NOTE
This is a fictional example of a SOAP note and should not be used for any medical or diagnostic purposes. Actual SOAP notes should be based on real patient data and follow appropriate documentation guidelines and standards.
Benefits and limitations
SOAP provides a widely recognized and accepted standard to record key information in a patient’s care plan. The format is easy to read and interpret, as the data is organized clearly and rationally. It also encourages the inclusion of all relevant details in a structured manner, thus promoting effective communication and coordination among healthcare providers.
However, SOAP notes can be time-consuming and tedious to prepare when nurses are busy. Also, if the nurse is incompetent, they may omit important data, leading to incomplete and substandard records. Lastly, SOAP notes are too rigid, preventing nurses from recording unique details, which can be crucial when treating a patient with complex medical needs or multiple comorbidities.
Summary
When giving patients nursing care in a hospital, clinic, or at home, you must take notes to record important information. Such notes record the patient’s medical status and interventions during a visit or encounter. However, they are also used to document the formulated care plan and track the patient’s progress in their treatment journey. It is important to read a few examples of the notes as a reference to ensure accuracy and completeness. Nursing notes should be shared with the health care team treating the patient on a need basis.