A General Medical History Form is a document used to record a patient’s medical history at the time of or after consultation and/or examination with a medical practitioner.
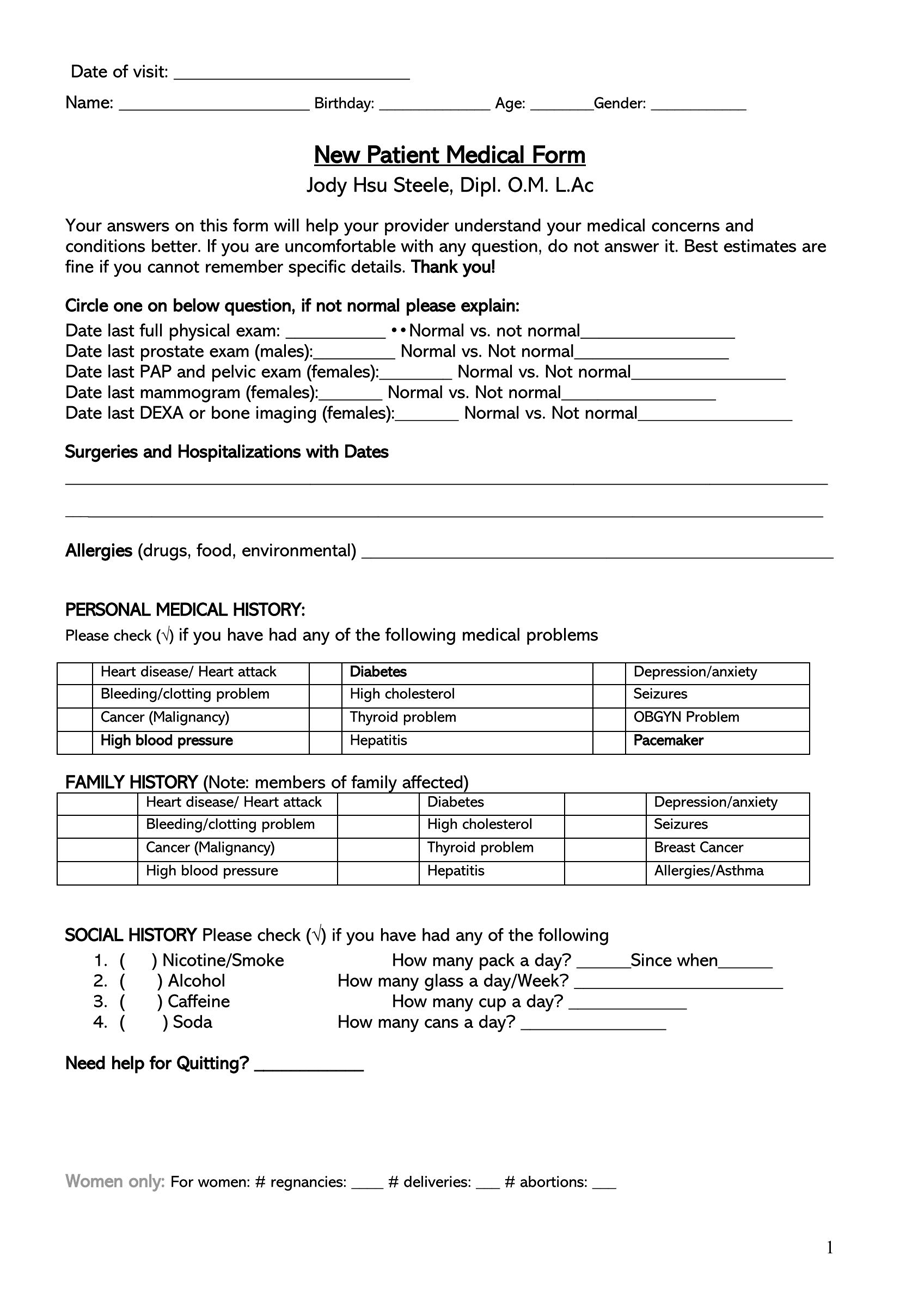
The form covers the patient’s personal medical history, such as diagnoses, medication, allergies, past diseases, therapies, clinical research, and that of their family.
A general medical history form is meant to document all relevant information regarding an individual’s health in order to act as a reference source or tool for any doctor diagnosing and making treatment decisions associated with the individual in question. Some of the records covered in it are past diagnoses, laboratory reports, doctor’s handwritten and typed notes, audiovisual records, and summaries of close family members’ reports.
Medical history forms are important communication tools between medical practitioners. Insurance providers also use them to review a patient’s health history to determine their insurability before offering health insurance coverage. Medical records are used to coordinate and combine existing knowledge of a patient’s medical care to provide effective and appropriate diagnoses and treatments.
General medical history forms simplify the process of recording and facilitate the availability of a patient’s medical information, as they can all be accessed from one place. With these in place, doctors are able to provide health care to a patient with risk factors and medical requirements taken into account.
Patients can also use their medical history forms to make healthy lifestyle changes and other interventions. For example, if cases of diabetes are common in family medical records, the patient can implement interventions that lower the risk of getting diabetes, such as low sugar intake and exercising often. They provide the doctor and patient with valuable information that can be used to guide healthcare decisions for the associated patient.
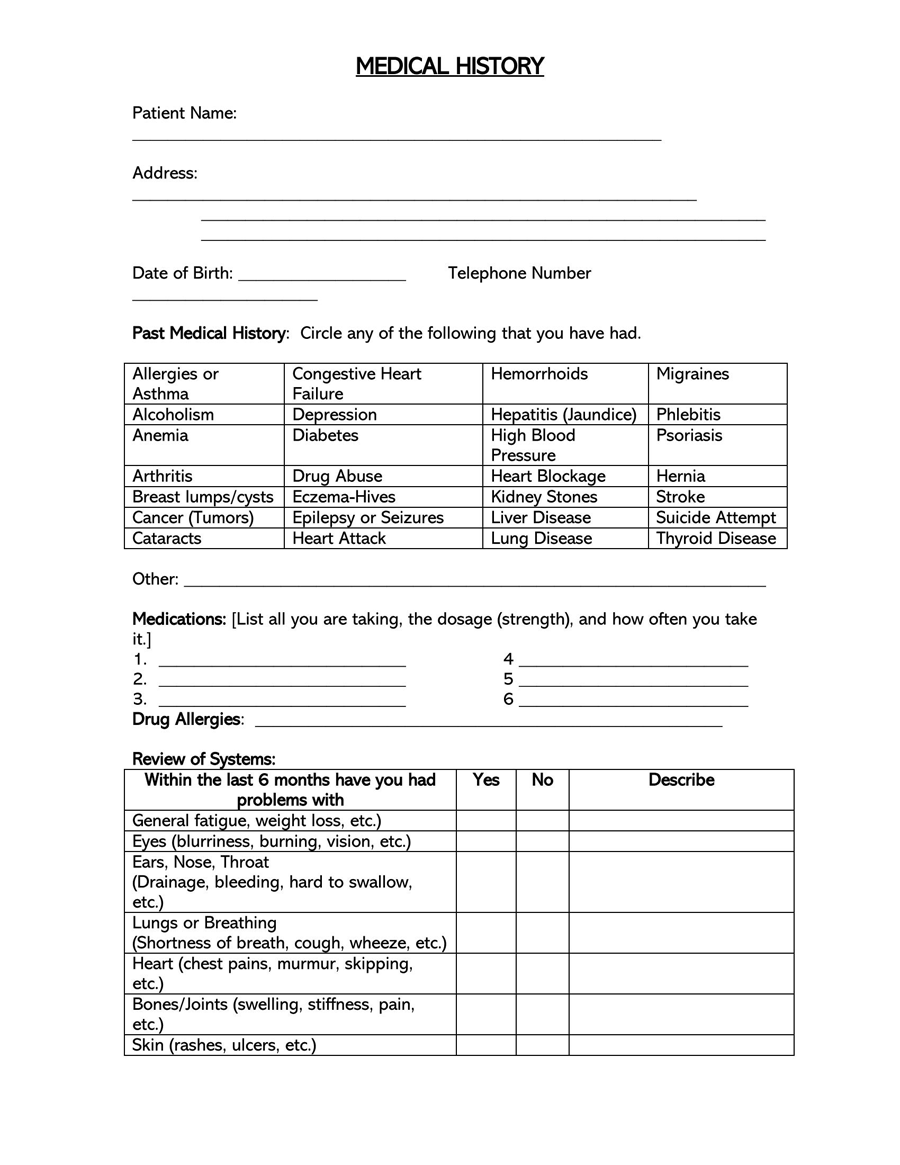
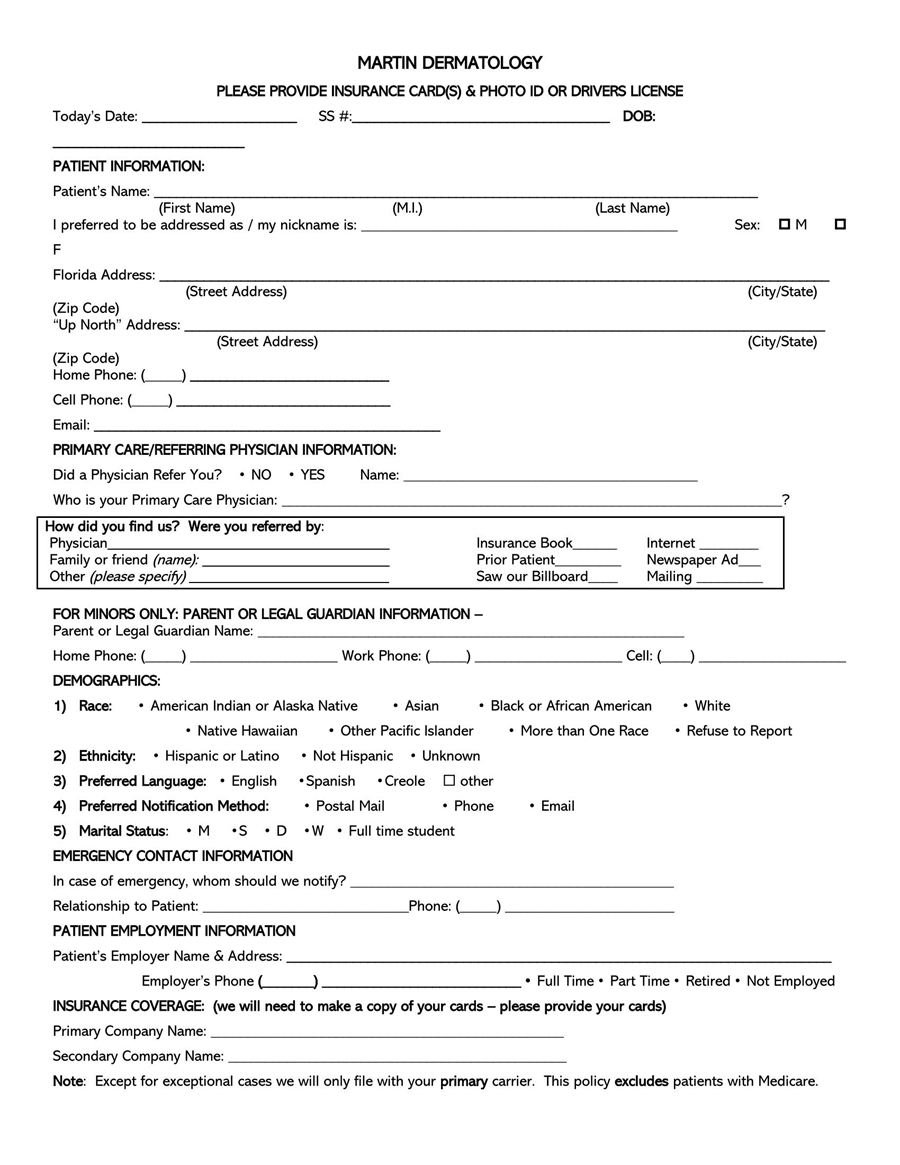
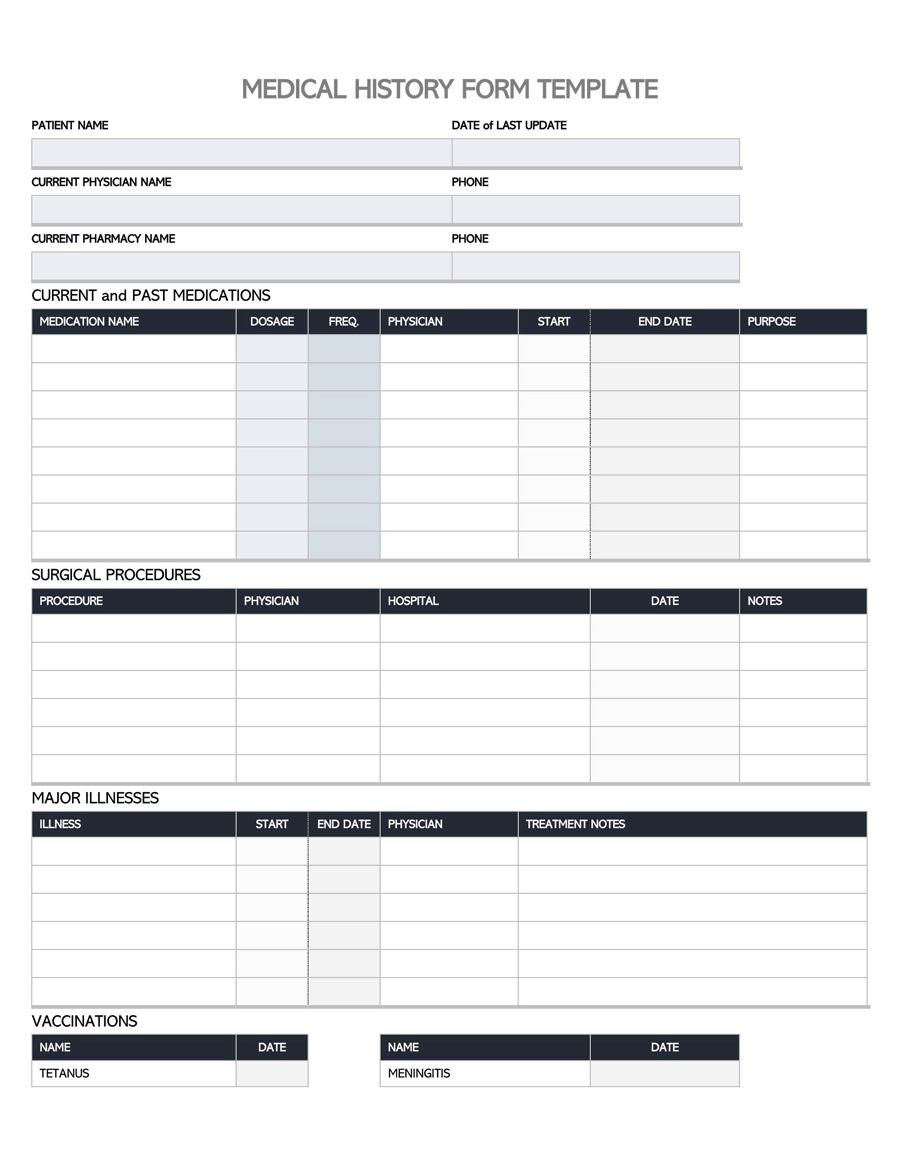
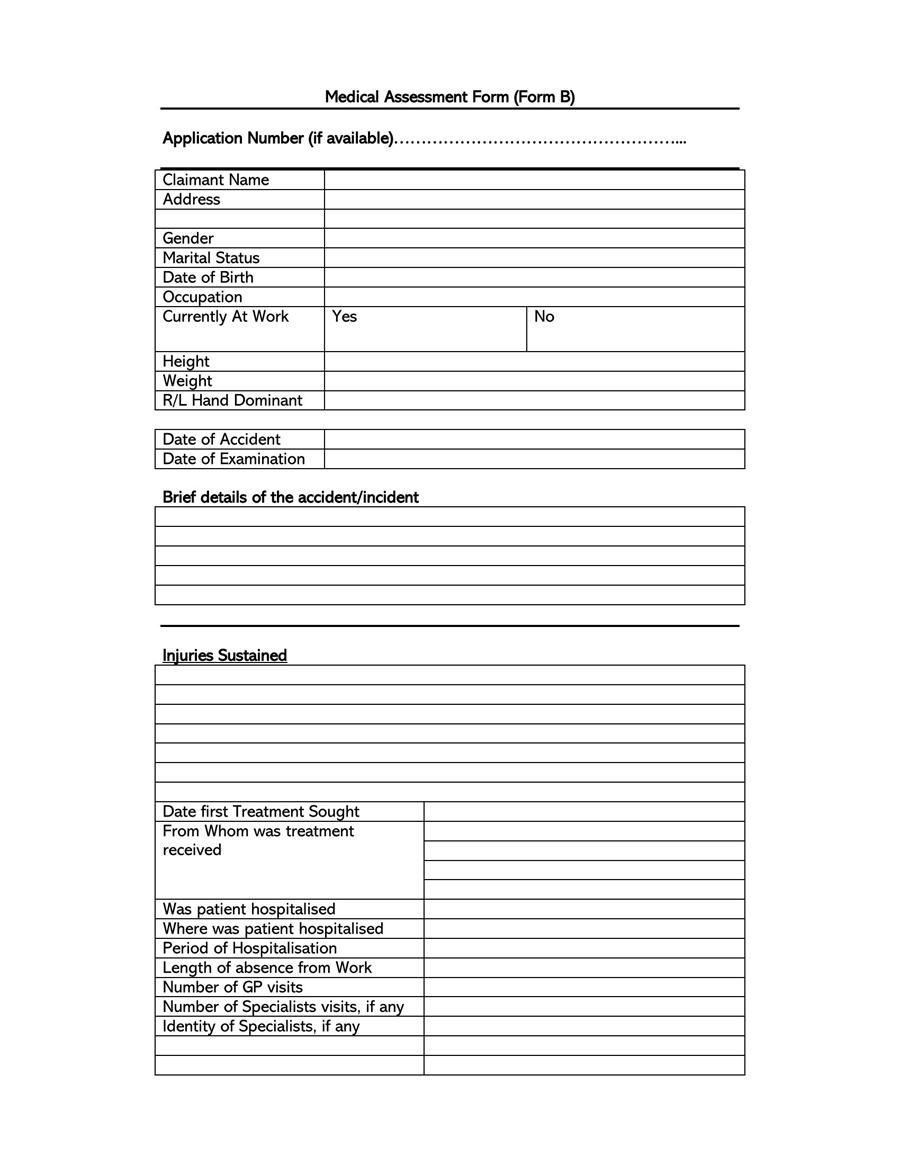
Downloadable Templates
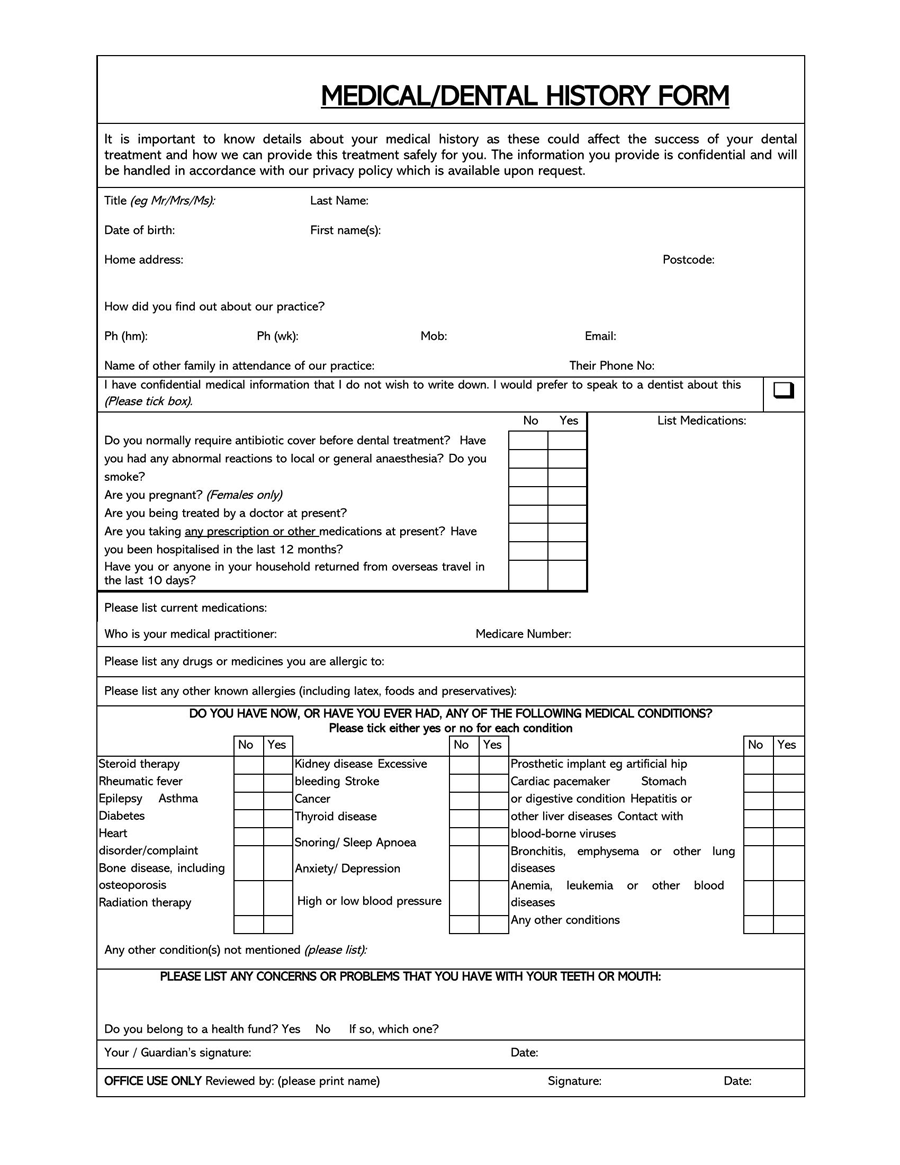
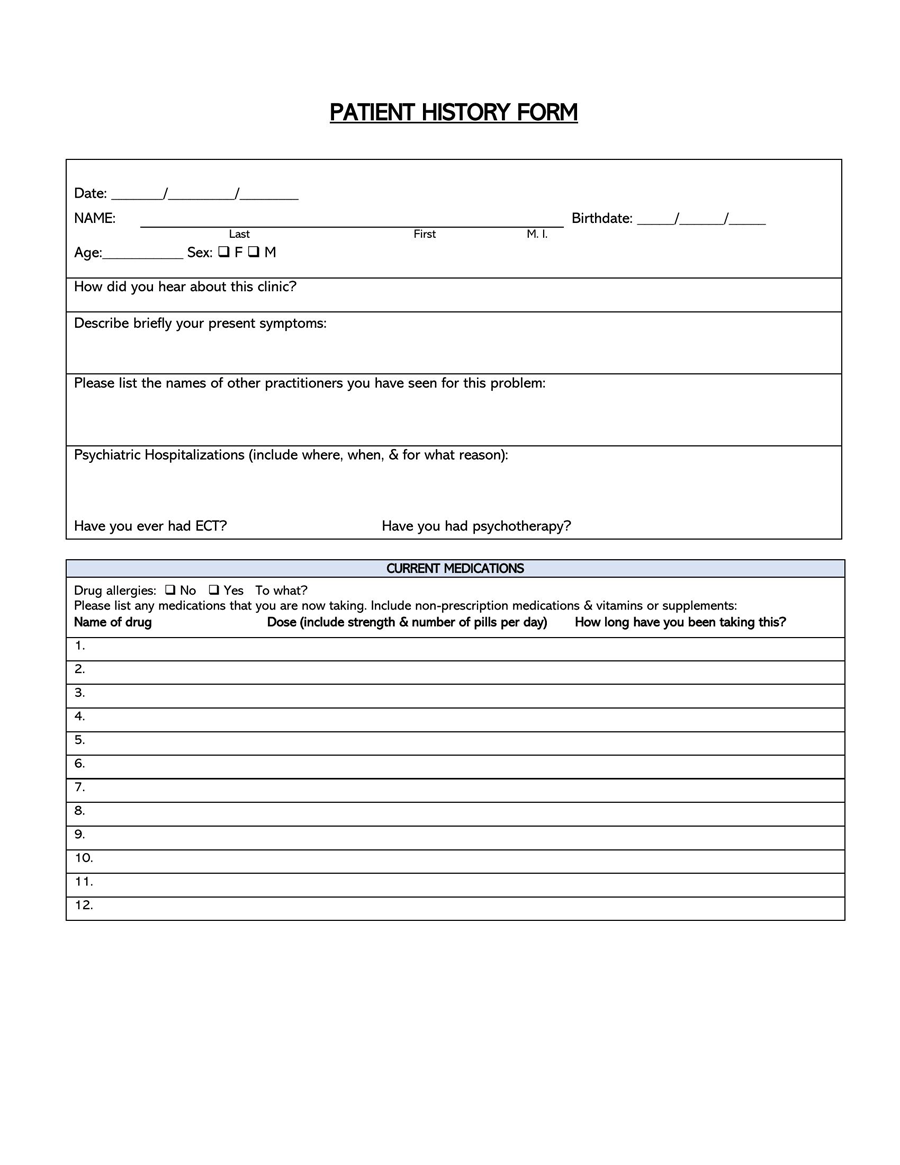
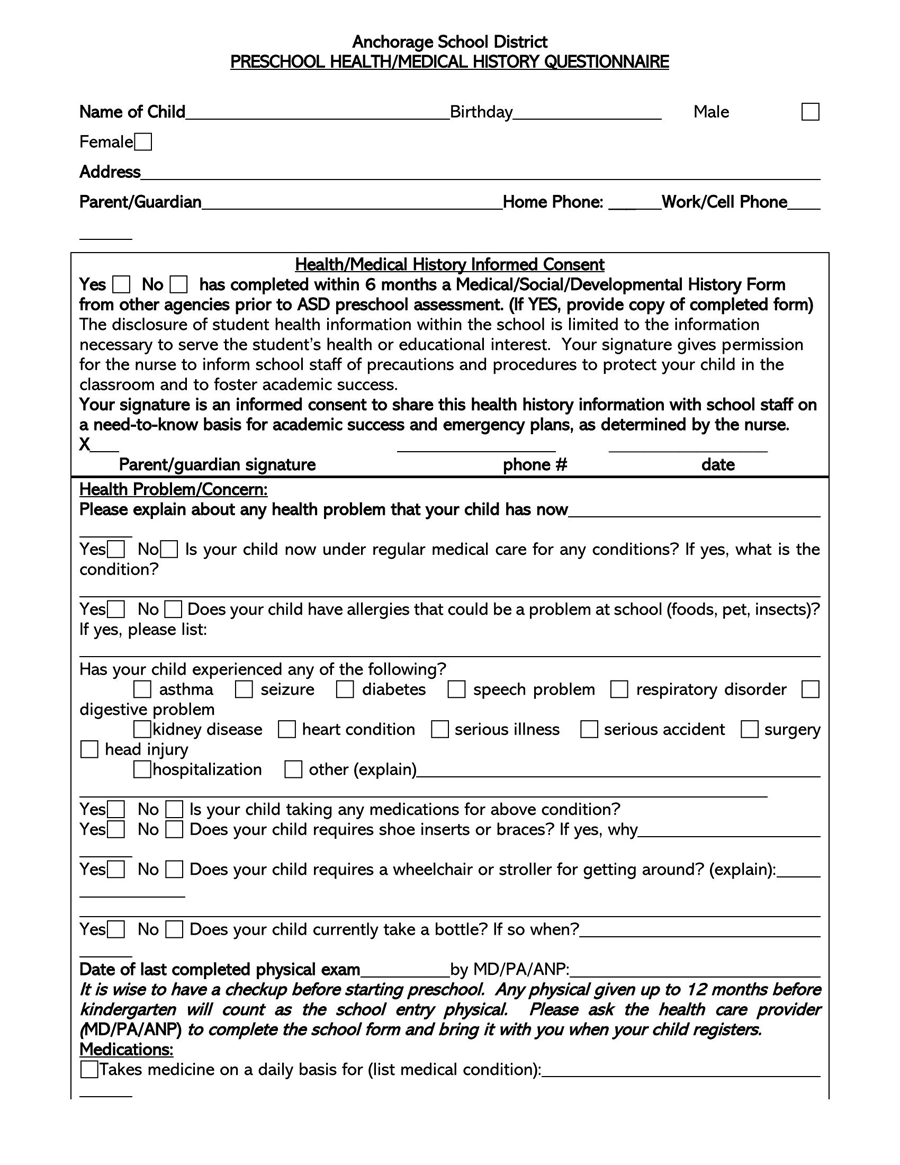
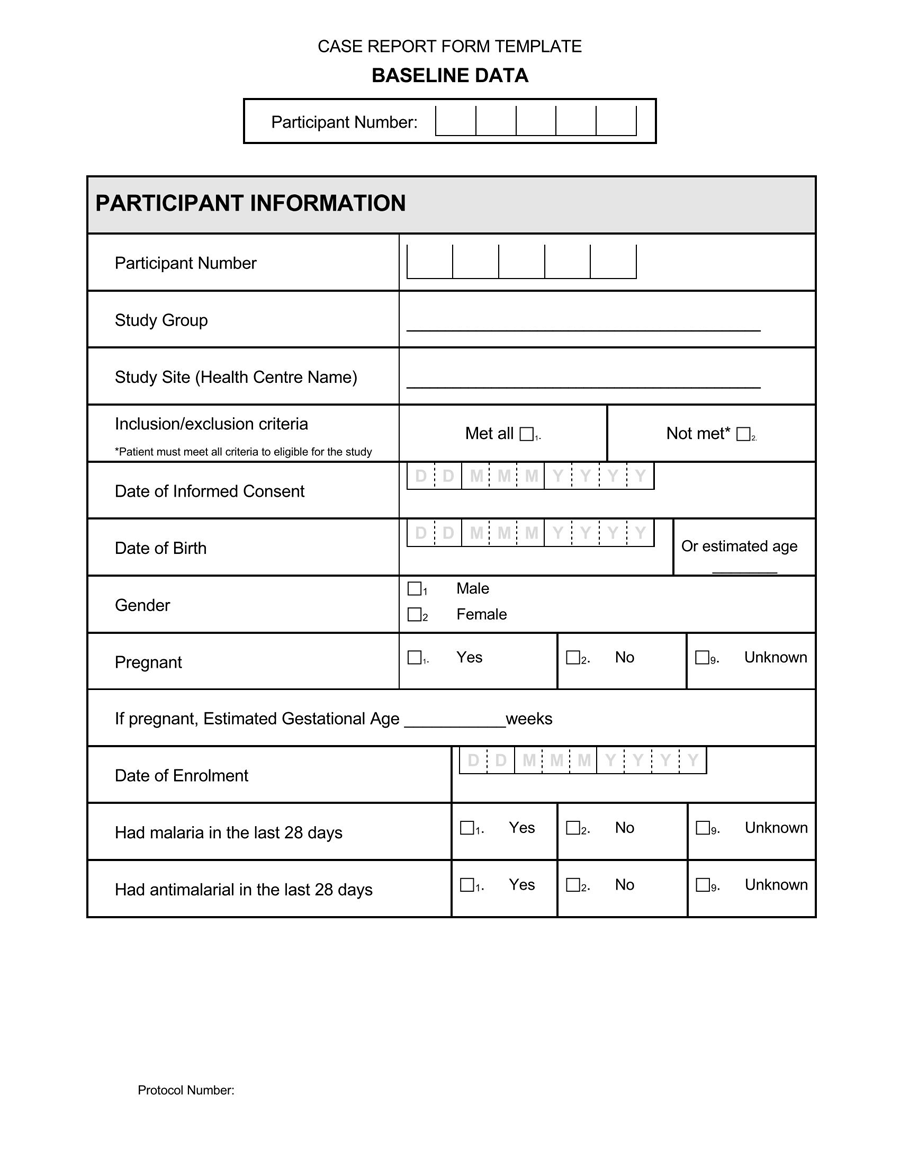
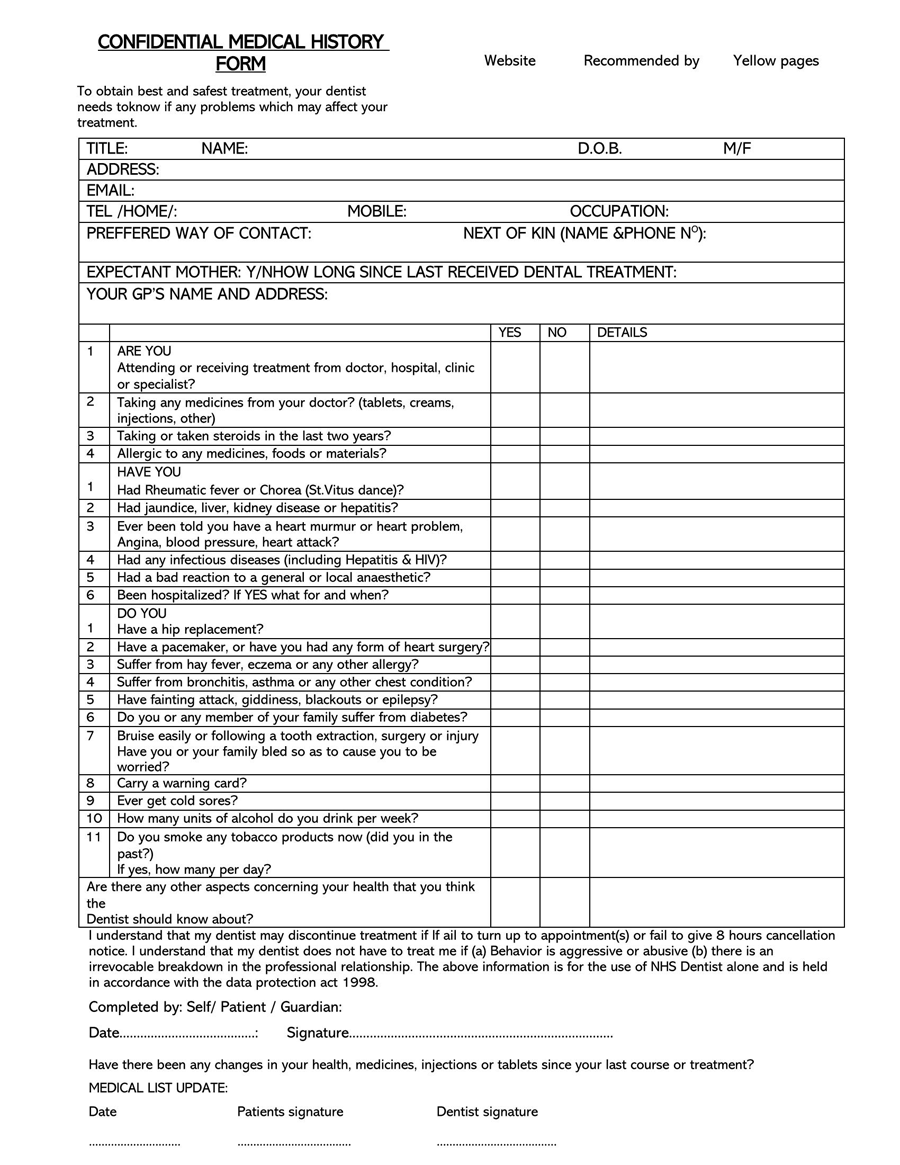
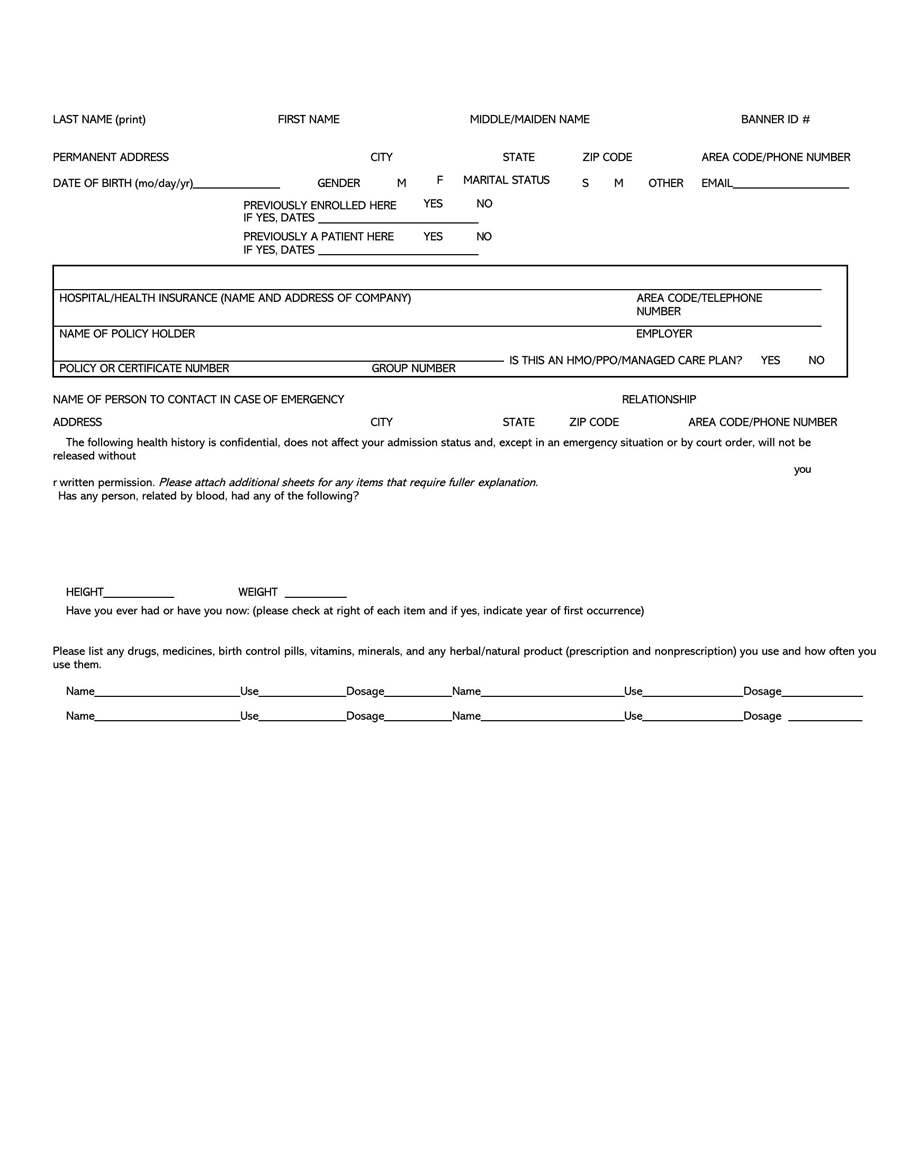
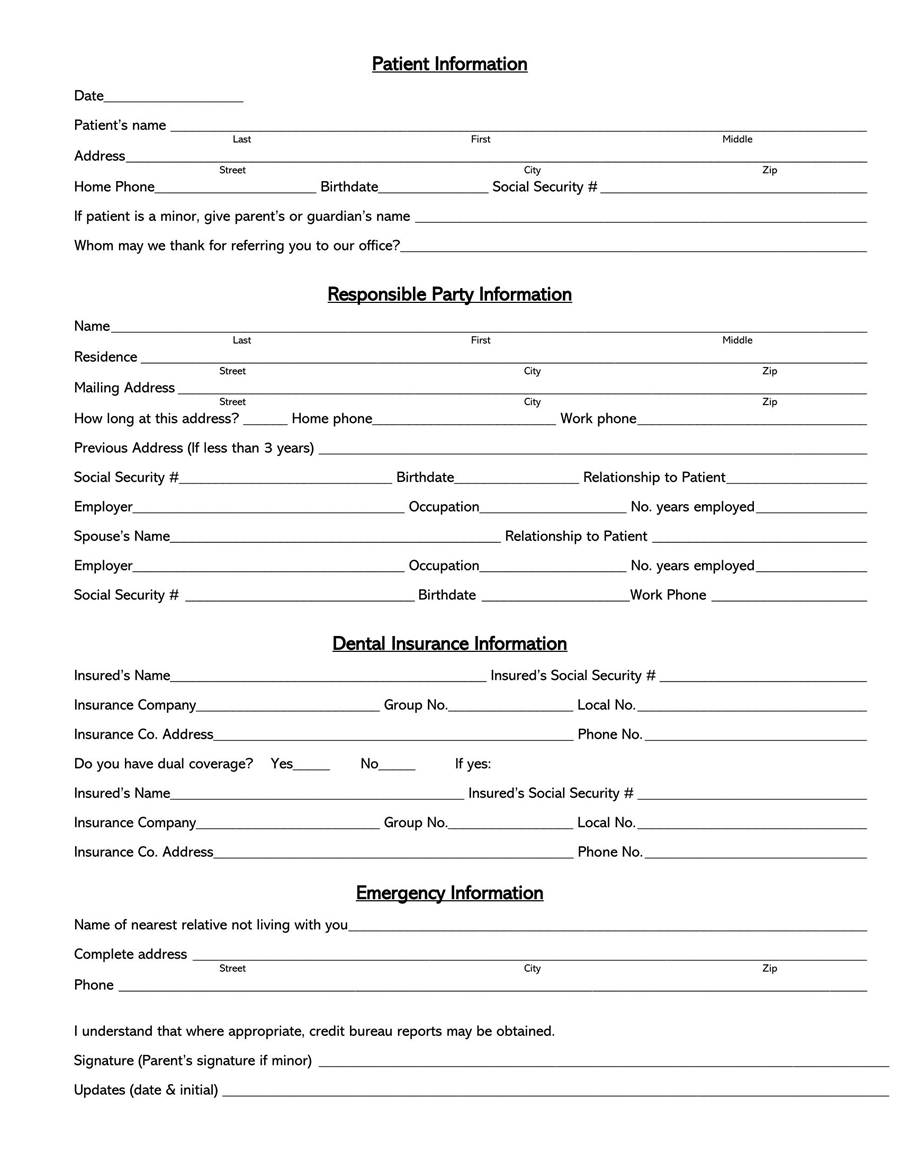
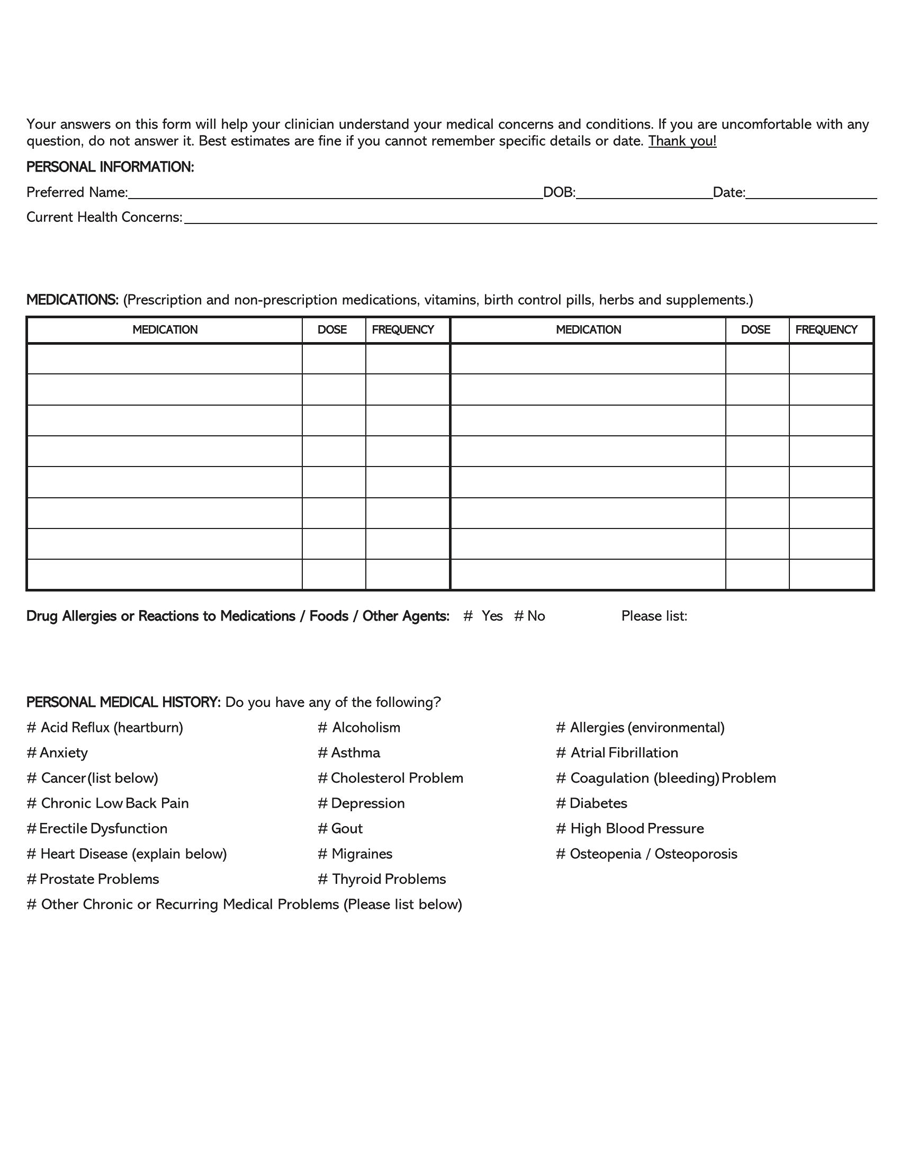
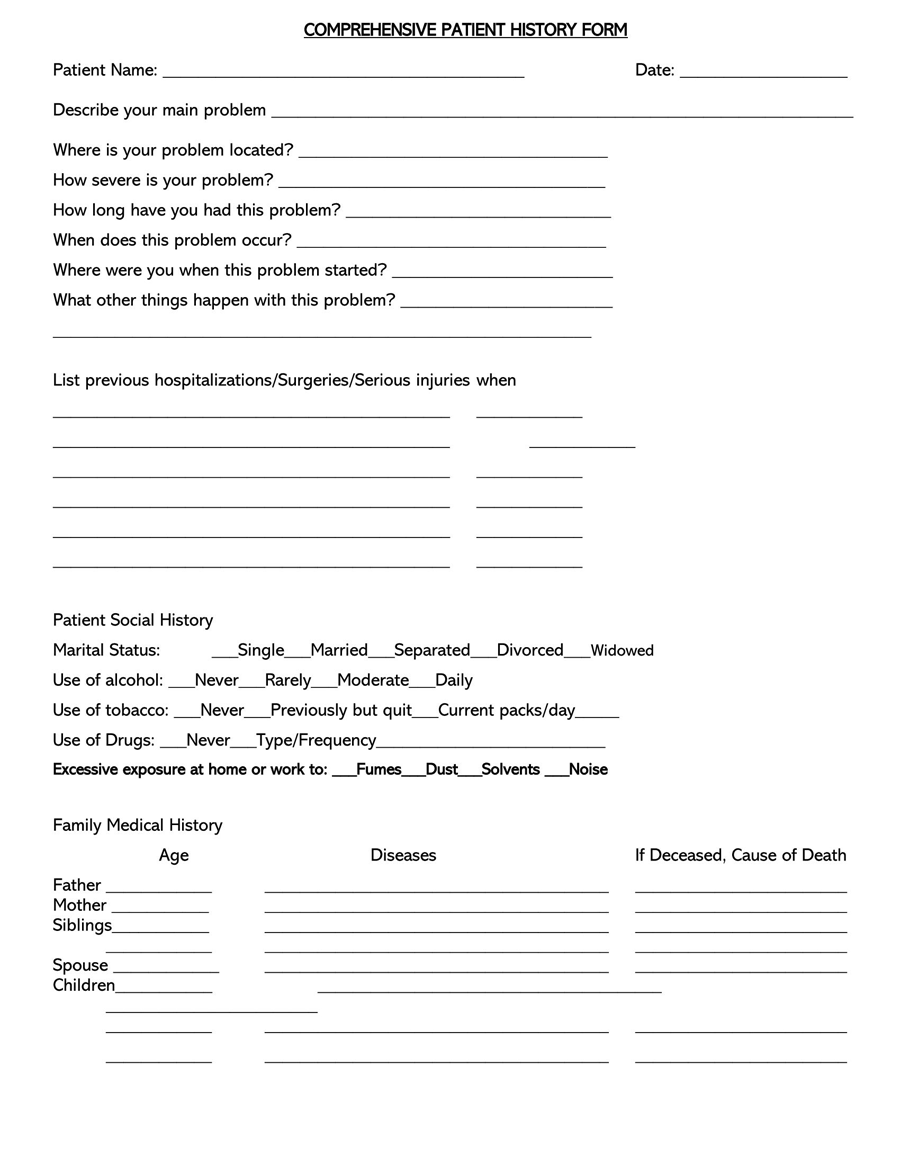
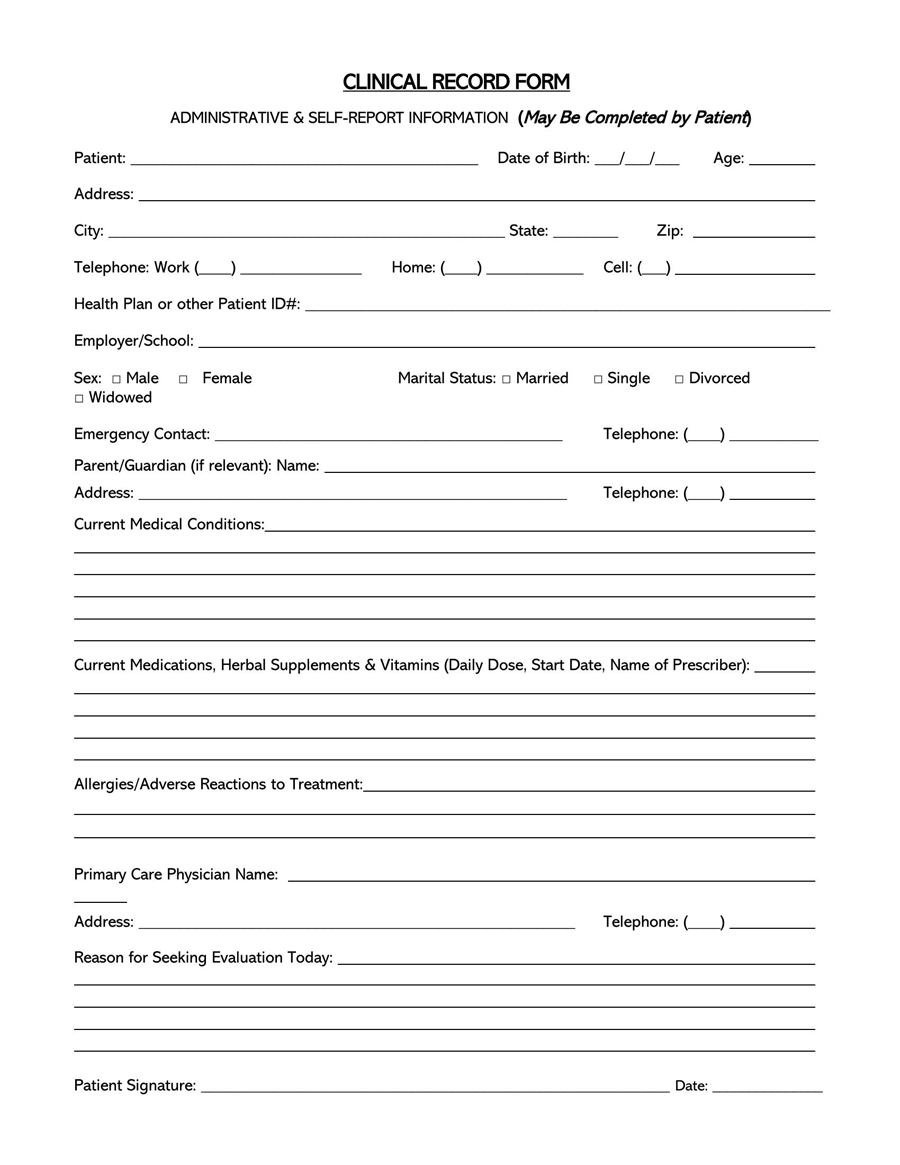
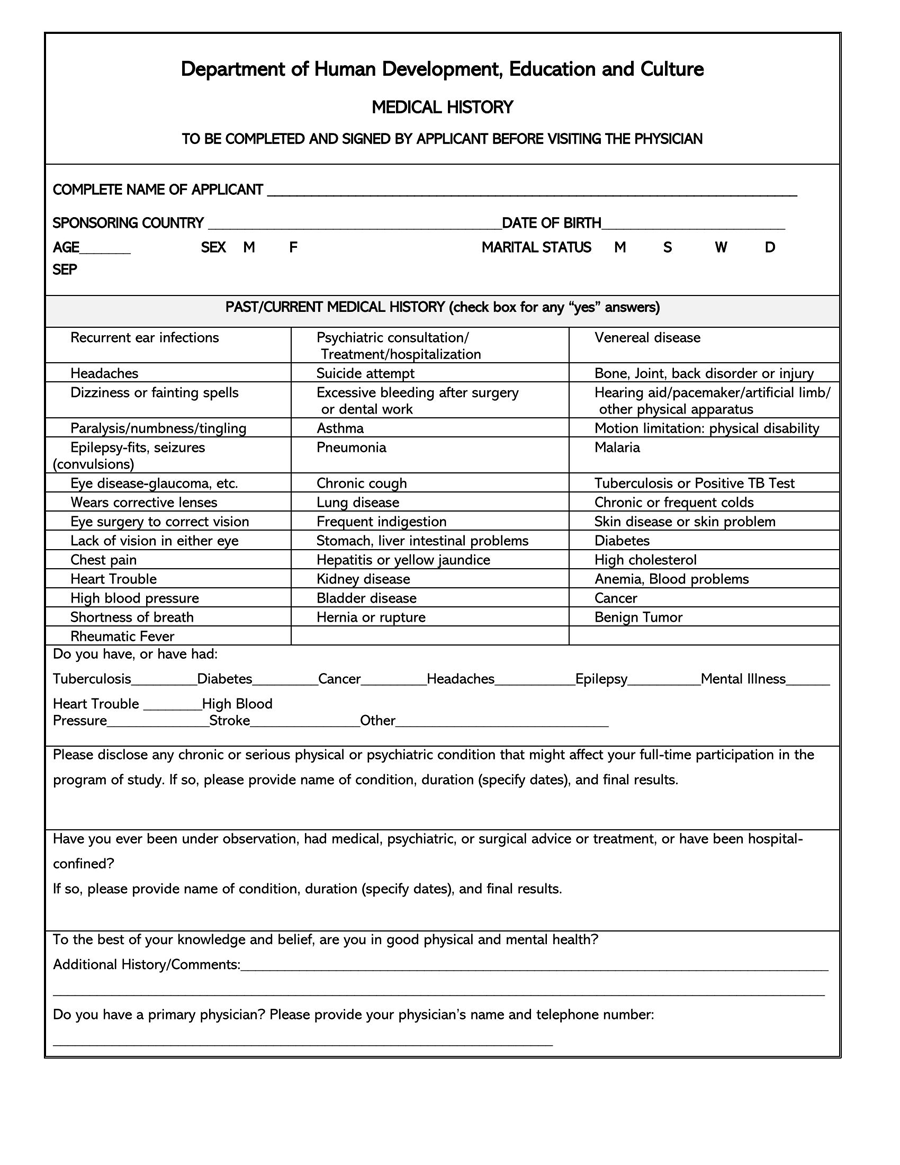
The design of general medical history forms will typically be unique to the associated medical center, even though they more or less request the same health care information. Therefore, templates can be used as guides to create health history forms. The templates are blank forms illustrating all the sections that should appear in a standard medical history record form. The templates are easily customizable to save the user time used to design and create their own form.
What Should be Included?
A general medical history form is not meant to replace the doctor’s file. Still, it should be comprehensive enough to give sufficient information to assist medical practitioners in making educated diagnoses and treatment decisions.
To achieve this, the following details should be captured in the document:
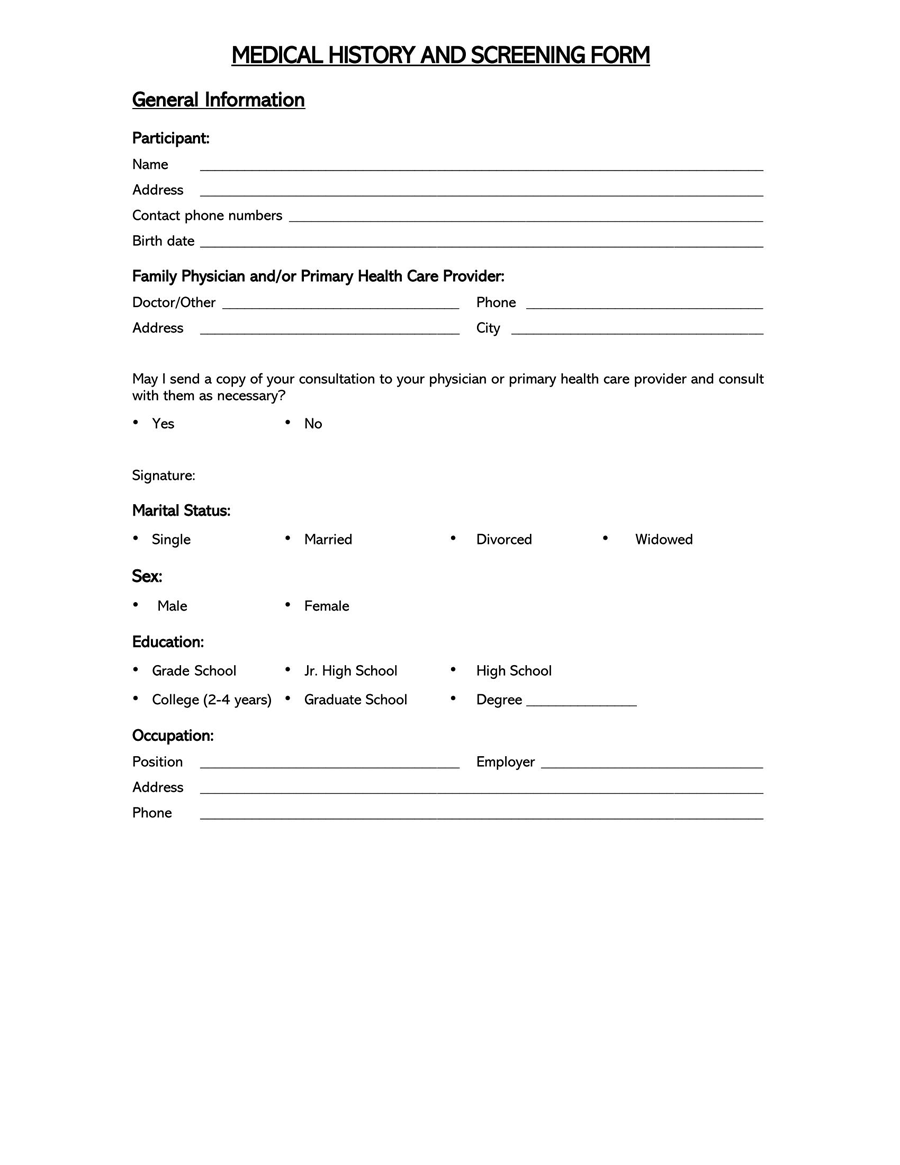
Patient’s personal details
Each form is unique to the associated patient. Therefore, the form should include personal identification such as name, date of birth, social security number, blood type, address, contact number, and email. This information can be utilized to identify the patient being referred to when medical records are being shared with multiple doctors.
Doctors’ details
The primary medical provider will typically store a patient’s health history form. It must therefore indicate the identification details of the doctor, which include name, address, and contact information such as contact number and email.
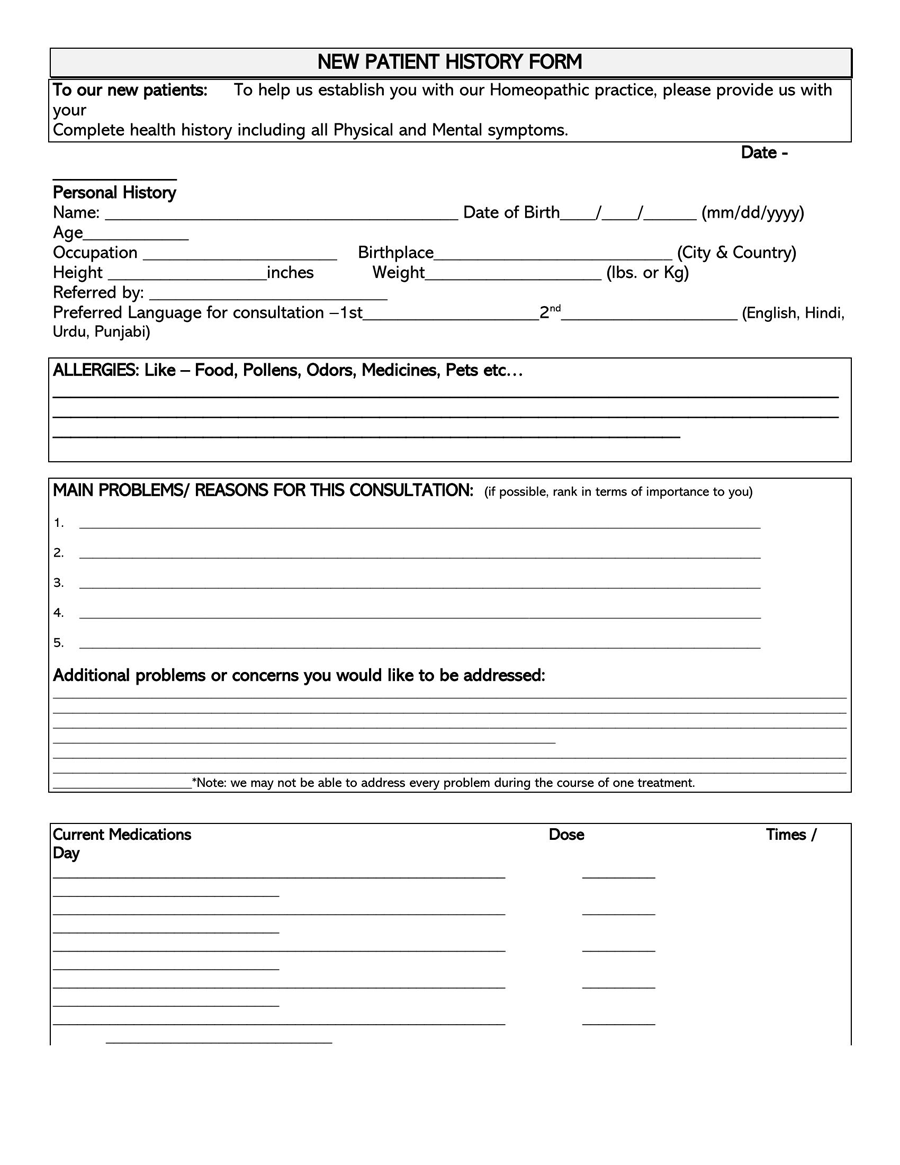
Details of the patient’s current problem and treatment
Since such a form will typically be filled out during a visit to the hospital or any other medical center, it must indicate the patient’s reason for the visit. This section should capture the following information:
- Time: The form must record the onset of the patient’s current problem. This is normally recorded as the date when the problem started. If the problem is recurring with no established pattern of occurrence, several dates may have to be recorded.
- Location: It must also be clear where the problem is occurring. For example, is the problem of pain in the heart, leg, or headache.
- List of all the symptoms: The medical history form should also list all the symptoms the patient is exhibiting. Symptoms are any undesirable, perceived changes to the normal functioning of the body. Common examples of symptoms associated with diseases or disorders are headache, fever, swelling, nausea, etc.
- Allergies: Allergies are any adverse reactions (hypersensitivity) to substances. People can be allergic to different substances and medications; it is imperative for the doctor to know these substances before making diagnoses and treatment recommendations.
- Current treatment: It should also indicate any treatments or remedies the patient is taking to address their problem. This includes prescribed and non-prescribed medications (over-the-counter drugs). The form should also state any other unrelated treatments the patient is undertaking, such as painkillers, supplements, diet tablets, suppressors, etc. This information is necessary, as some medications are dangerous when mixed with other drugs.
- Change in routine: The form must also indicate any changes in the patient’s lifestyle, as some medical problems may result from these changes and not necessarily diseases. State any unusual activities, such as travel, new exercise routine, manual duties undertaken, and diet changes implemented in the last few months.
- Your health concerns: The patient should also record what they think is the problem in their words. This subjective information provides the doctor with the starting point for diagnosing the patient.
Patient’s past medical history
The form should cover the patient’s previous medical details. These can be records of previous visits, examinations, symptoms, and other medical information.
It should record the following details of the patient’s past medical history:
- Past health problems and surgeries: The patient should indicate any major health problems they have had and surgeries they have undergone previously.
- Systemic diseases: The health history form needs to state any existing or previous systematic diseases the patient may have had. Systematic diseases affect the entire body rather than one organ or part of the body. Examples of systematic diseases are flu, high blood pressure, stroke, etc.
- Medications: A patient can also indicate any medication they are currently taking from previous diagnoses and what medications did not suit them in the past.
- Herbal supplements: It should list any herbal supplements the patient may be using. Herbal supplements are substances or products obtained from plants and their extracts, such as oils, seeds, flowers, etc.
- Diagnostic tests: The medical history form must also include any health care diagnostic tests done on the individual. This includes blood tests, X-rays, mammograms, genetic tests, biopsies, etc.
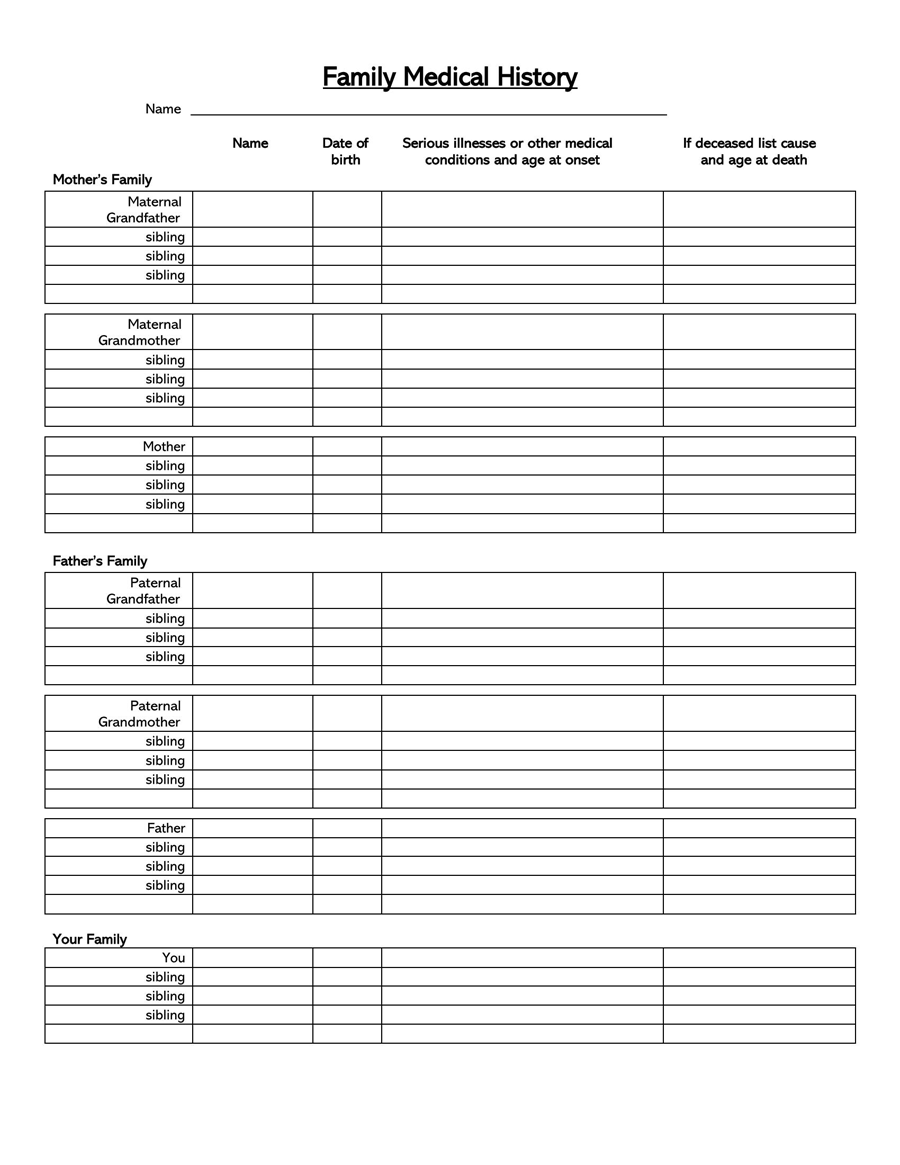
The patient’s family medical history
The patient’s family medical history is essential for educated diagnoses. The patient needs to include any prevalent conditions, diseases, and medical complications prevalent in the family line. Only blood relatives such as parents, siblings, blood cousins, aunts, and uncles need to be indicated.
NOTE
Relatives such as in-laws, spouses, adopted relatives, and step-siblings should not be considered family.
The patient’s recent health screenings
It should indicate the patient’s recent health screenings. This section should capture the accurate dates and what the individual was screened for.
Social behaviors that can potentially influence a patient’s health should also be stated. This includes behaviors such as smoking, alcohol drinking, occupations that would expose the patient to harmful substances, etc.
Immunizations
It should also indicate the different immunizations an individual has taken. This information is important for eliminating the probability of certain diseases, such as tetanus, that individuals can be vaccinated against.
Reaction to anesthetics, if any
A medical history form allows patients to indicate if they react negatively to anesthetics. Anesthetics are drugs induced to reduce pain and are common for surgical operations. This information helps the doctor be prepared for what to avoid should surgical interventions be necessary.
Patient’s insurance information
Medical insurance is a huge consideration for doctors when treating patients. Patients are therefore required to input their medical insurance details, such as the type of insurance coverage and the name of the insurer, in a health care history form.
Patient’s questions and expectations
Patients are also allowed to write down any questions they might have for the doctor and their expectations regarding the appointment. Some common questions are when the examination results can be expected and after how long the patient should contact the doctor if no improvements are observed. If the examination is a requirement for another process, such as an appointment for a position, any required documentation from the doctor can be requested in this section.
Doctor’s progress notes
A comprehensive form should record the doctor’s progress notes. This section is where any updates and changes to medication, recommendations, and treatments can be recorded.
The next item that should appear is the doctor’s follow-up remarks. This section will normally be completed once the patient follows up with their doctor after the initial visit.
Additional information to include
A medical history form should capture as much information as possible to assist the doctor or individual in reviewing the document to get a detailed overview of the patient’s health. This will often require recording additional information such as blood type, allergies to foods, lifestyle habits, a list of names of other medical care providers and specialists, and emergency contacts.
Delivery option
Patients should also state their preferred delivery method if the doctor is to send the document to the patient, for example, before the next appointment. For online medical records, the document will usually be available in the patient’s portal. However, it can be mailed or emailed too.
Signatures
It is important that both the patient and their doctor sign the medical history document. They should sign the document at the end to ensure that the privacy of the document under HIPAA (Health Insurance Portability and Accounting Act) is protected.
NOTE
The crucial sections or highly significant information that patients have to fill should be marked with an attention-grabbing tool such as a label, sticker, or notation. This ensures no important information is overlooked.
Who Can Benefit from a Medical History Form?
General medical history forms are utilized by a variety of parties, not just doctors. Below are the people who can benefit from it and the different ways this is possible.
They include;
Doctor/medical staff
Doctors and medical staff attending to a patient use the form to determine their health history before intervening. From this, doctors can make informed diagnoses and collect supporting information for their evaluations. On the other hand, medical staff such as nurses can provide better health care to the patient; this can be immensely important in emergencies and in-patient cases.
Parents
Parents typically complete such forms for their children and will consequently have access to them. By doing so, they are able to see the doctor’s notes regarding the child. They can then use the information in the forms to monitor their children’s health.
Insurance companies
Insurance firms are common users of this document. It will ordinarily be a requirement when customers are applying for health insurance with an insurer. The insurance firm reviews the document to determine their insurability and prevent a situation where they assume more liability than they can cope with.
Psychiatrist
Psychiatrists use such records during psychiatric evaluations. Psychiatrists will often use health history forms associated with psychiatric and mental health records. Psychiatric history forms will typically be lengthy and more detailed, containing details of previous psychiatric examinations.
General physician
General physicians also make examinations and diagnoses based on a patient’s medical history. Therefore, they will require patients to complete such forms before making any interventions. They are often presented as questionnaires where patients are required to answer yes-or-no questions.
Caregiver or advocate
Caregivers and advocates can also use general medical history forms to conduct their assigned obligations. However, they will usually have to present a completed authorization form signed by the patient in this case. Caregivers use this information to ensure they give quality health care to the patients, while advocates will usually use it for legal matters such as proof of incapacitation.
Frequently Asked Questions
Patients will always be required to fill it out before or when they visit the doctor for outpatients and before being admitted for inpatients. This can be done at home or in a hospital before they see the doctor. The forms are updated when the doctor makes diagnoses, prescribes medication for the current problem, and after follow-ups and subsequent visits. At the very least, the form should be updated once a year.
They can be formatted in any way that ensures they are readily accessible, easily portable, and tightly secure (medical records are sensitive records whose privacy has to be prioritized, especially from third parties other than the doctor or authorized family members). The form can thus be in PDF, spreadsheet, or notebook.
The family’s medical history is important in identifying inheritable conditions and diseases, even if non-existent at the moment. In addition to this, providing this information helps the doctor make recommendations for reducing the risk of the identified diseases and conditions. When a patient learns their family medical history, they are also able to note early signs of the disease and conditions, which play a crucial role in prevention rather than cure when a problem is identified in the early stages.
Ordinarily, a patient will have to wait thirty to sixty days after requesting their medical history. The waiting period will vary from one doctor/institution to another, but the legal limits are dictated by state laws, which differ from state to state. Requesting it involves a written or typed request for the medical institution or doctor.
The access to medical history form is governed by HIPAA regulations and varies from one situation to another. HIPAA allows the patient, the patient’s guardian (for minors), caregivers, and advocates with written permission from the patient to access this information. Note that there are also limitations as to what medical information the named parties can access.
Other parties allowed to access a patient’s medical records are the primary healthcare provider and entities such as insurance firms, rehabilitation centers, nursing homes, hospitals, labs, etc. Mobile app companies are also examples of entities that patients can allow to access their medical information through a formal request by the patient or by signing up.