Documentation of the problem is the first and most important part in the process of providing professional patient care. Accurate documentation results in improved and effective treatment plans and methods. That is when a SOAP note proves to be beneficial.
The note was first introduced into the medical field by Dr. Lawrence Weed in the early 1970s and was referred to as the Problem-Oriented Medical Record (POMR). At the time, there was no standardized process for medical documentation. These notes provide the physician’s structure and a way for them to easily communicate with each other, which is still helping transform the industry.
Healthcare professionals widely use these notes to document patient information in healthcare facilities and consider them significantly effective. It is a document that contains the chronological details of a patient’s journey throughout their treatment. It is considered legally credible in several scenarios where it provides evidence of the healthcare treatment given to a patient.
Healthcare professionals use the notes to record important information based on the different stages of a patient’s treatment. They serve as highly effective communication tools between their own teams and healthcare professionals from other facilities involved in the treatment.
Professionals consider these notes to have significant legal credibility and importance as they are proof of the patient’s treatment.
Furthermore, your patients might essentially require them for insurance-related purposes after receiving treatment from you. Health insurance is widely popular, and most individuals who attain healthcare services are conscious of it, as some people might not afford extensive healthcare costs.
The usage of the notes extends beyond the primary care facet of the healthcare system. Rather, healthcare professionals belonging to different fields utilize it. For instance, those in the field of psychiatry, as well as social sciences. We will discuss these types, along with the other necessary factors associated with SOAP notes in detail with examples in this article.
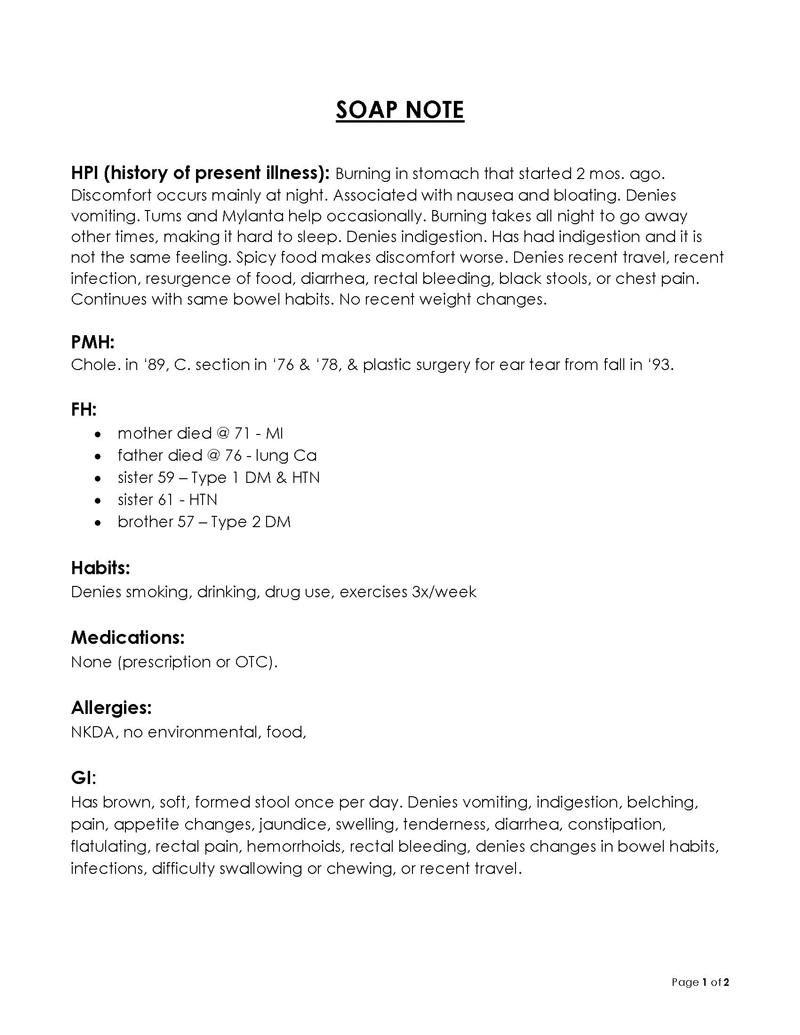
Soap Note Examples
What is SOAP Note and How to Make It
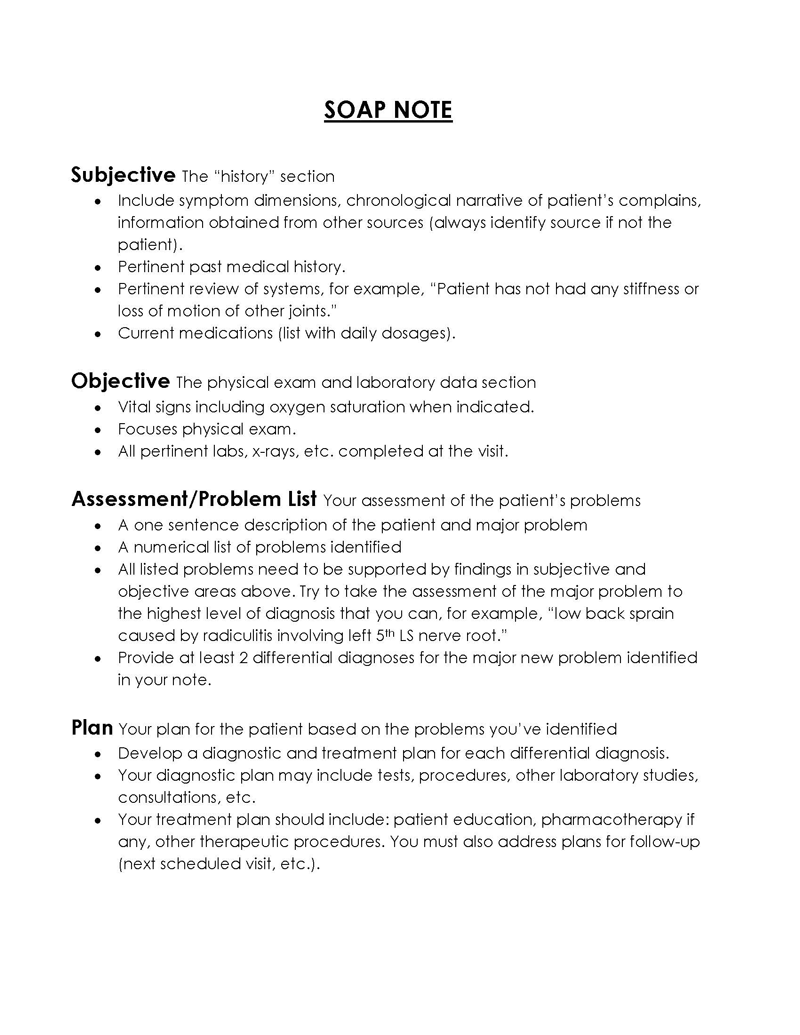
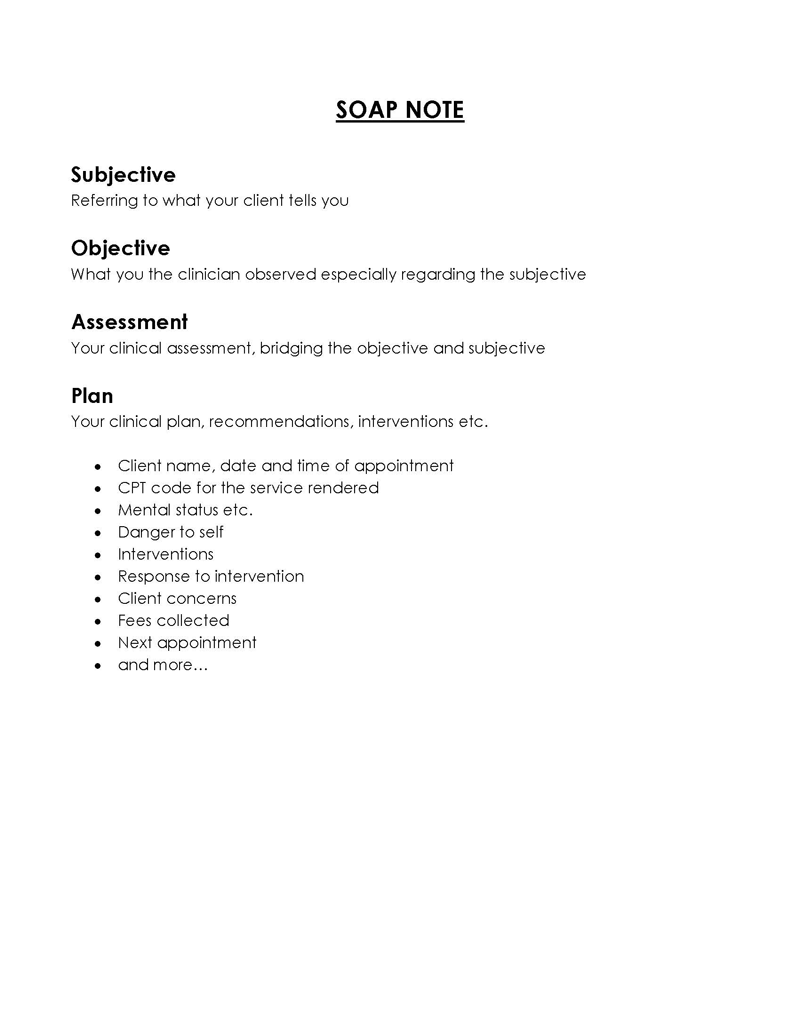
SOAP is basically an acronym for Subjective, Objective, Assessment, and Plan. In medical terms, it is a systematic framework or approach toward the documentation and continual management of a patient’s problem(s) during their healthcare or treatment plan.
Each of the 4 aforementioned aspects that make up the note or diagram details different categories of information.
We discuss the segments of SOAP in detail for you below:
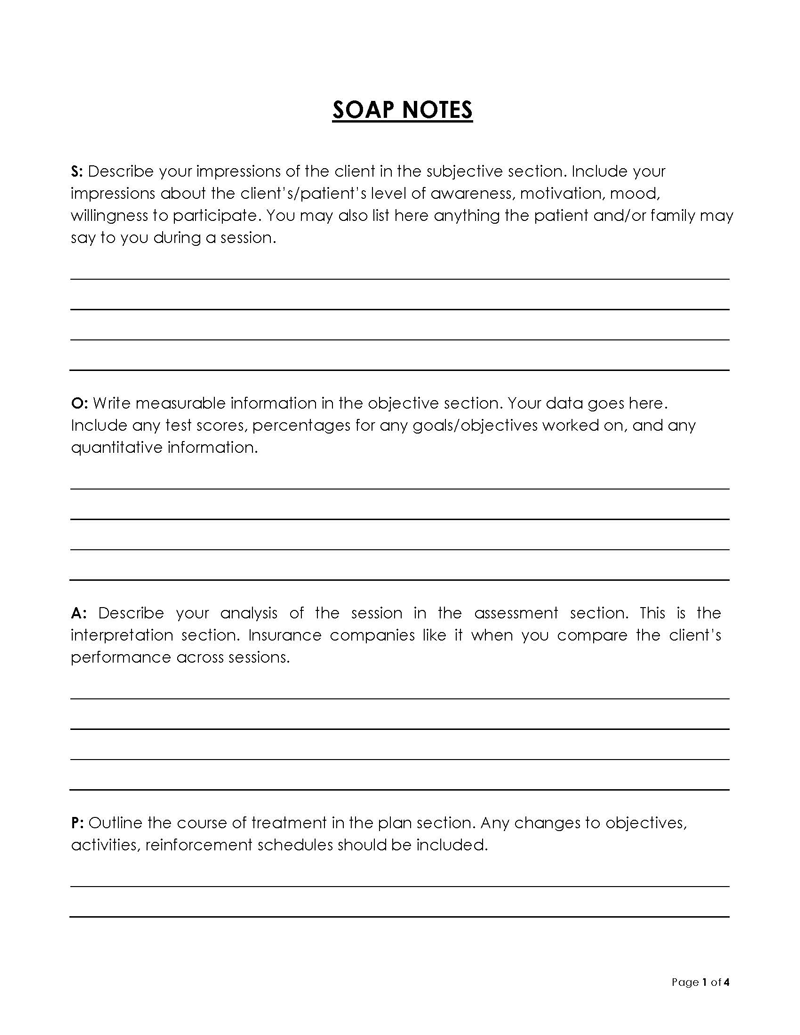
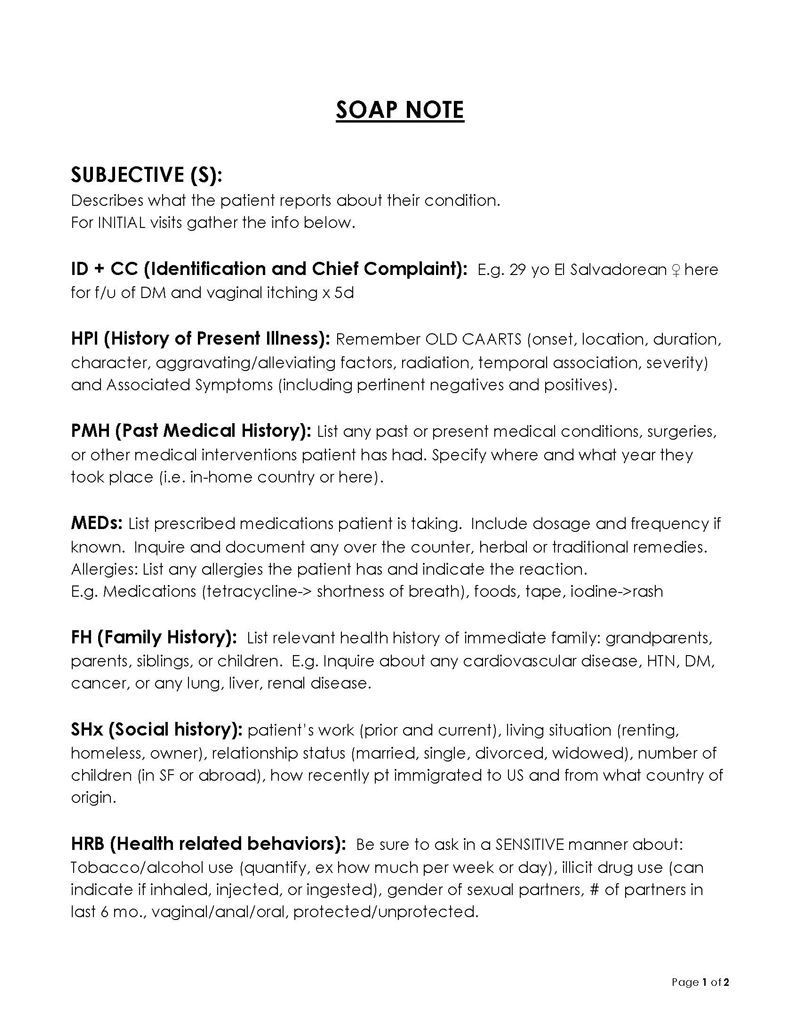
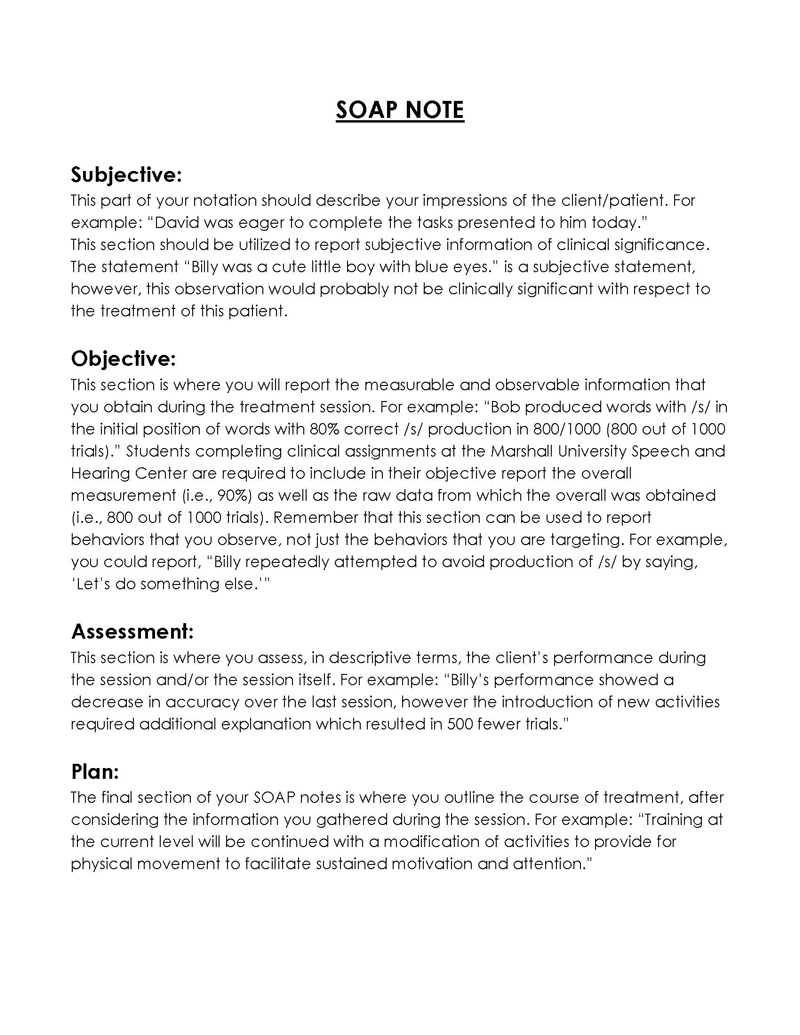
“S” for subjective
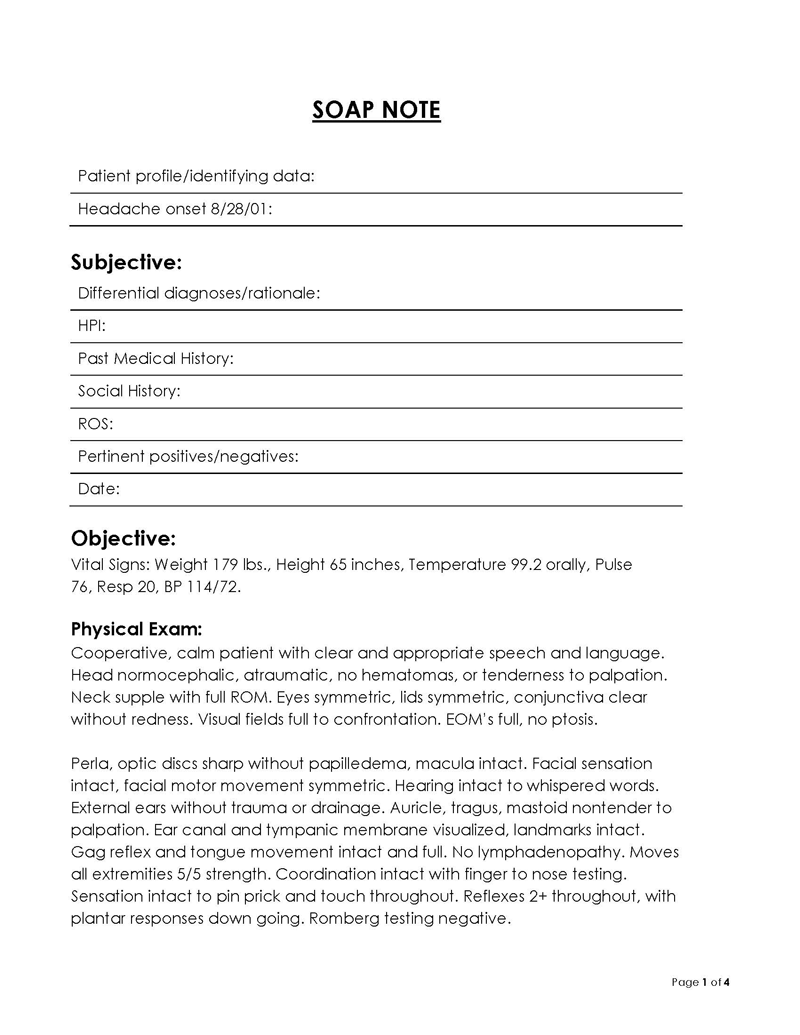
In the context of the notes, the “S” or “Subjective” component relates to the patient’s verbal statements based on their self-assessment of their condition.
This section might typically discuss their condition in terms of their symptoms, onset, duration, severity, location and/or concerns based on their medical history. The patient’s last visit to a healthcare specialist due to their medical condition would also be relevant here.
Furthermore, the healthcare professional must also contribute to this section with their own subjective assessment of certain factors relating to the condition of the patient in question. These could include lifestyle habits, emotional state, and social history, etc.
Note that in this section, you can also document the subjective approach of the patient’s family members and/or direct caregivers.
Documenting the factors of subjective assessment essentially helps healthcare professionals gather the insight to form the foundation for the next section of the note, in which they propose suitable treatment plans based on current conditions.
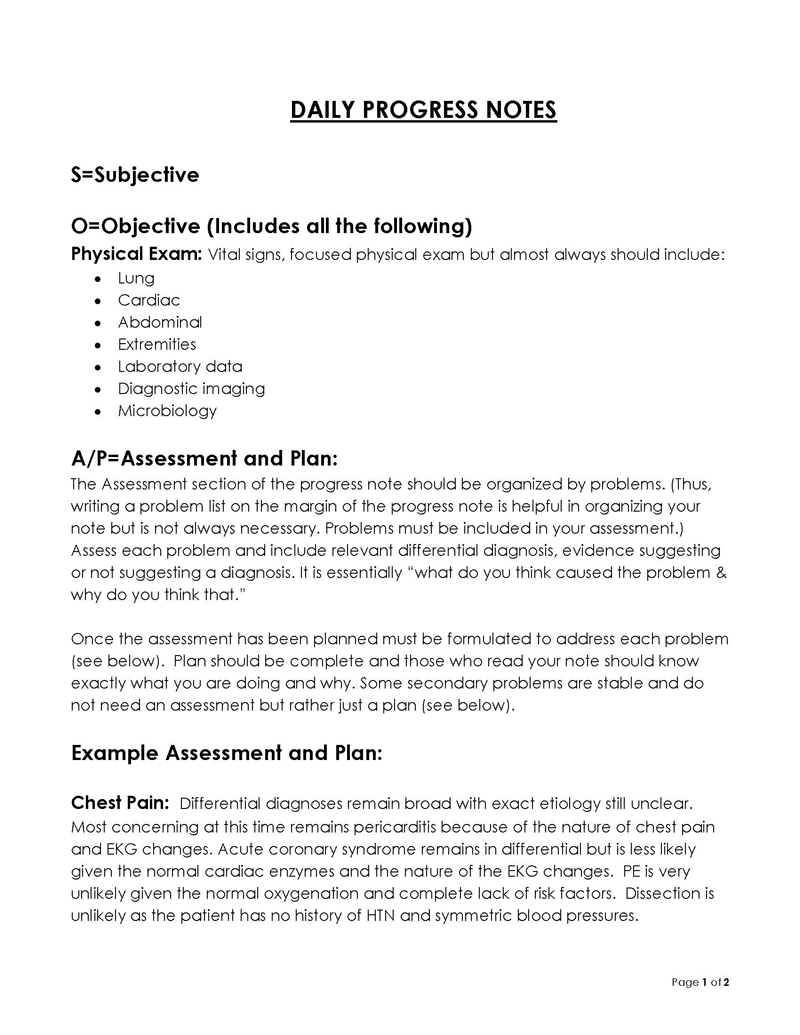
“O” for objective
The section of the notes focusing on “objective” statements, as the name suggests, details the factual information of the patient’s condition based on physical examination and/or diagnostic test results, etc.
Here, you document the quantifiable data to administer further treatment(s).
For example, it would include vital signs data (blood sugar, blood pressure, pulse, respiratory rate), physical examination findings such as response, palpitation, auscultation, and/or laboratory or imaging test results if relevant.
note
The major difference between a “subjective” and “objective” statement in the note is that its subjective section documents “symptoms”, for example; “stomachache” whereas the objective section discusses “signs”; e.g “abdominal tenderness and sensitivity to touch”. The former is a description/assessment from the patient’s perspective, and the latter is the medical professional’s specific assessment.
“A” for assessment
In this component of the note, you focus on developing diagnoses based on the collaborative findings of the subjective and objective sections. It is also considered the most important part of it due to its legal credibility, as it is the medical professional’s formal conclusion about the case’s condition.
When the objective and subjective findings are interconnected in this section, they form as basis for additional possible causes behind the patient’s condition. Typically, this element of the notes contains two parts.
Examples and definitions:
- Problem: Here, the medical professional lists the problems faced by the patient in terms of priority or severity and, therefore, importance.
EXAMPLE
Miss sarah; a 52 year old presented to the emergency room with severe abdominal pains in her lower right quadrant and has reported recent vomiting after consumption of food.
- Differential diagnosis: After enlisting the major problems, you assess their inter-relatedness in terms of possible causes and diagnoses. You do this usually by considering the most likely to least likely diagnoses based on your medical knowledge.
EXAMPLE
Patient reports family history of IBD. Patients must be admitted and be considered and checked for IBD symptoms and tests, appendicitis, kidney stone, or gastrointestinal infection.
Furthermore, the assessment element of the notes also details the severity of the patient’s current conditions and includes the proposed or recommended treatment plan or actions.
note
The recommendations in this section could also simply be guidance tips by the doctor or therapist for the patient’s caregivers or family members. This is usually in cases when the condition is not too dangerous for the patient.
“P” for plan
In the last part based on the “P” factor of these notes, suggest the follow-up plan. This can be directed to either the other medical practitioners within the same facility, or for external specialists. In it, you draw a conclusion of the aforementioned aspects of the patient’s condition and discuss the practical steps to take next.
EXAMPLE
Diagnostic tests required for clear understanding of the cause of ailment. Admission is also prescribed until the patient regains comfort with orally ingesting medicine rather than taking it through intravenous methods.” Intravenous painkillers are also prescribed until the patients regain comfort with oral ingestion of medicine.
This section also essentially helps other physicians that the patient might consult in the near or distant future. It improves the factor of continuity in their treatment.
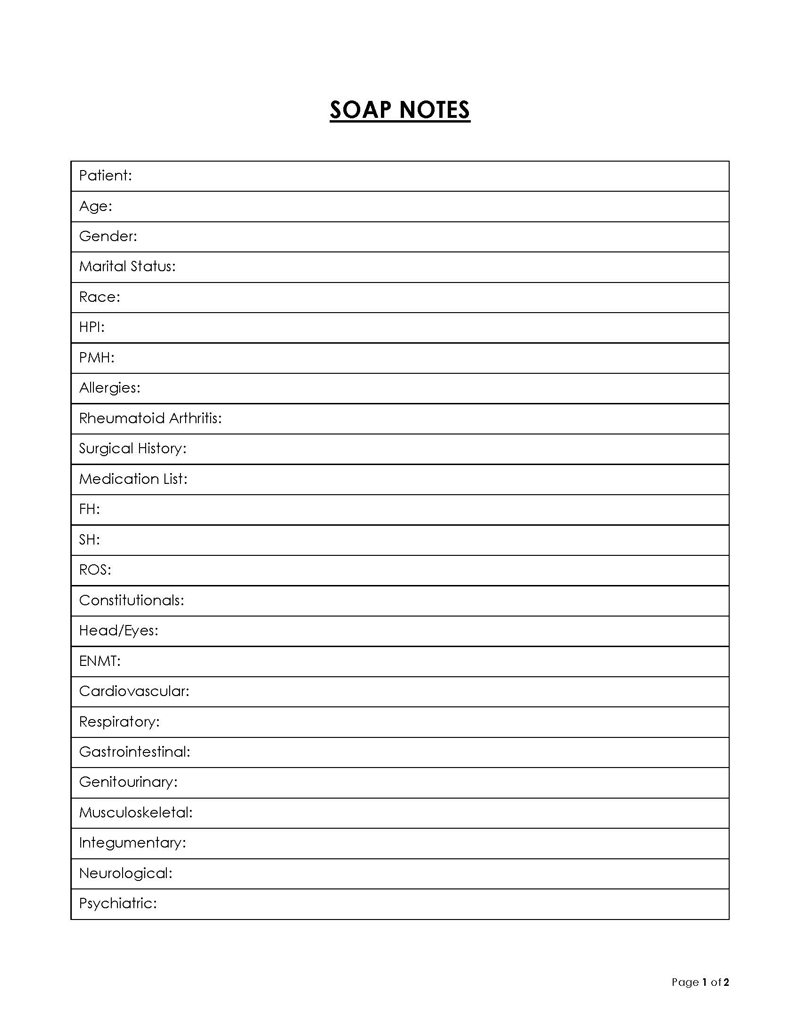
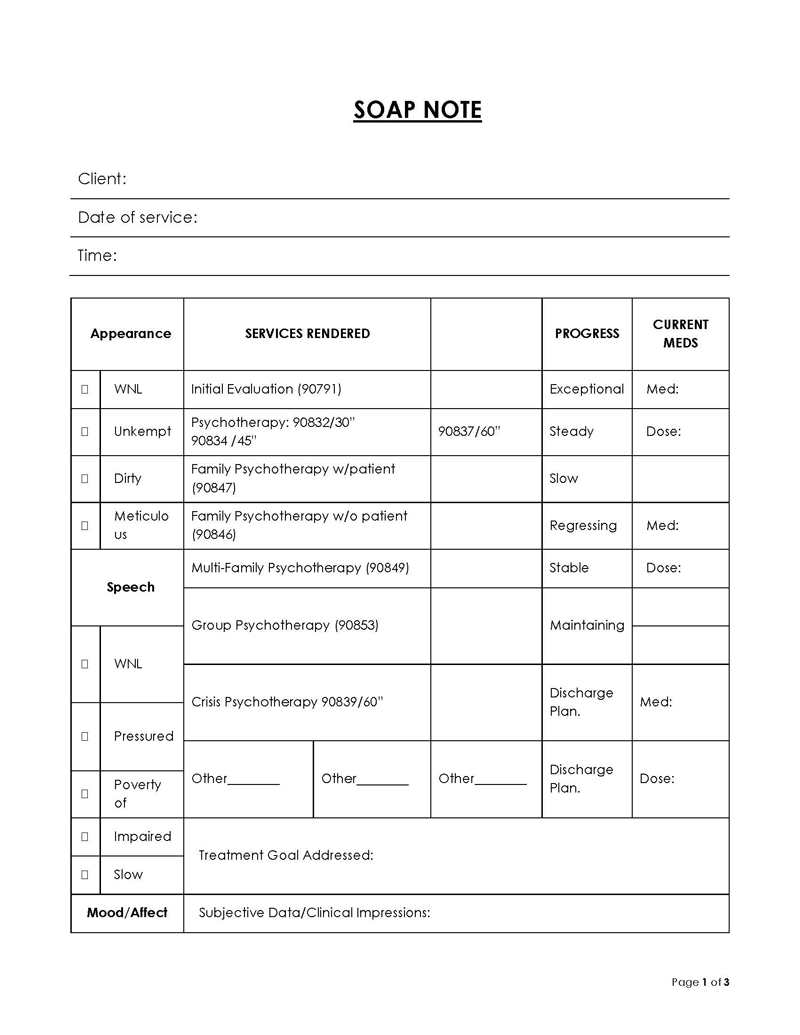
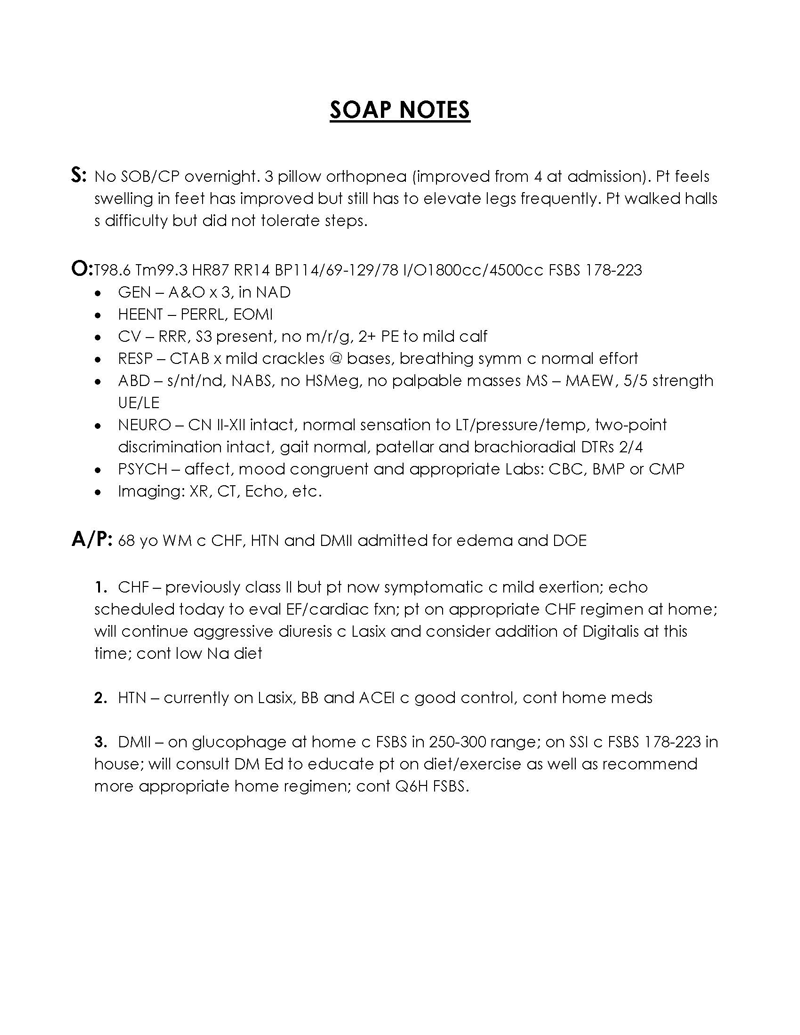
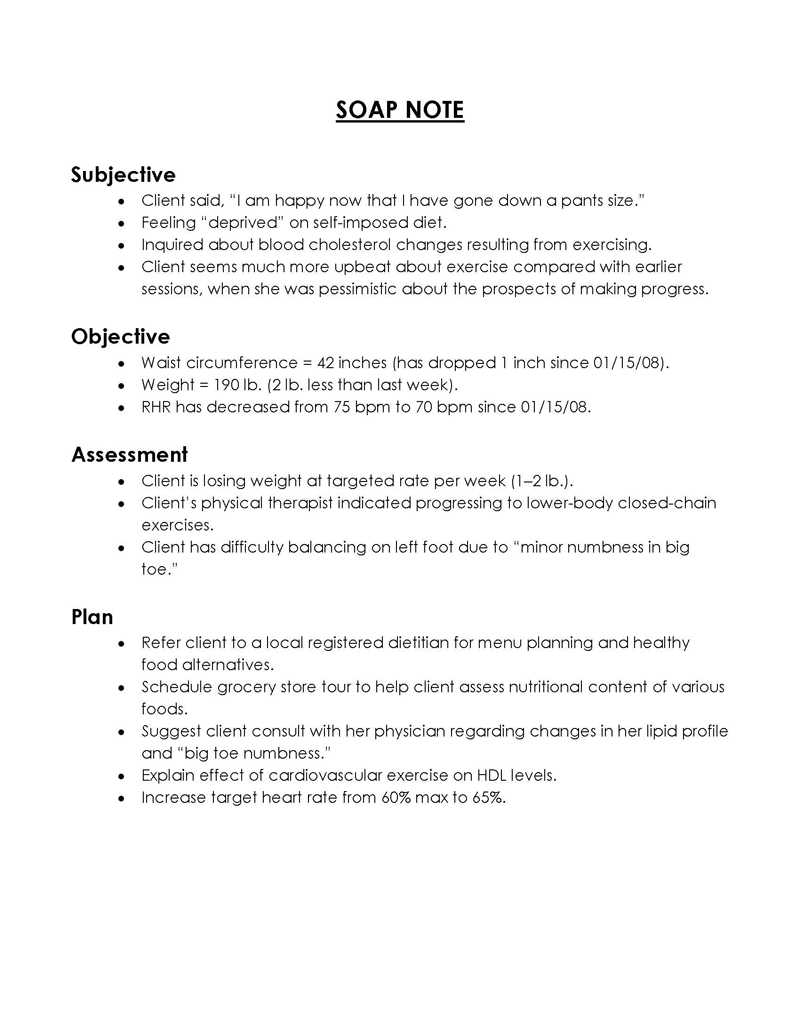
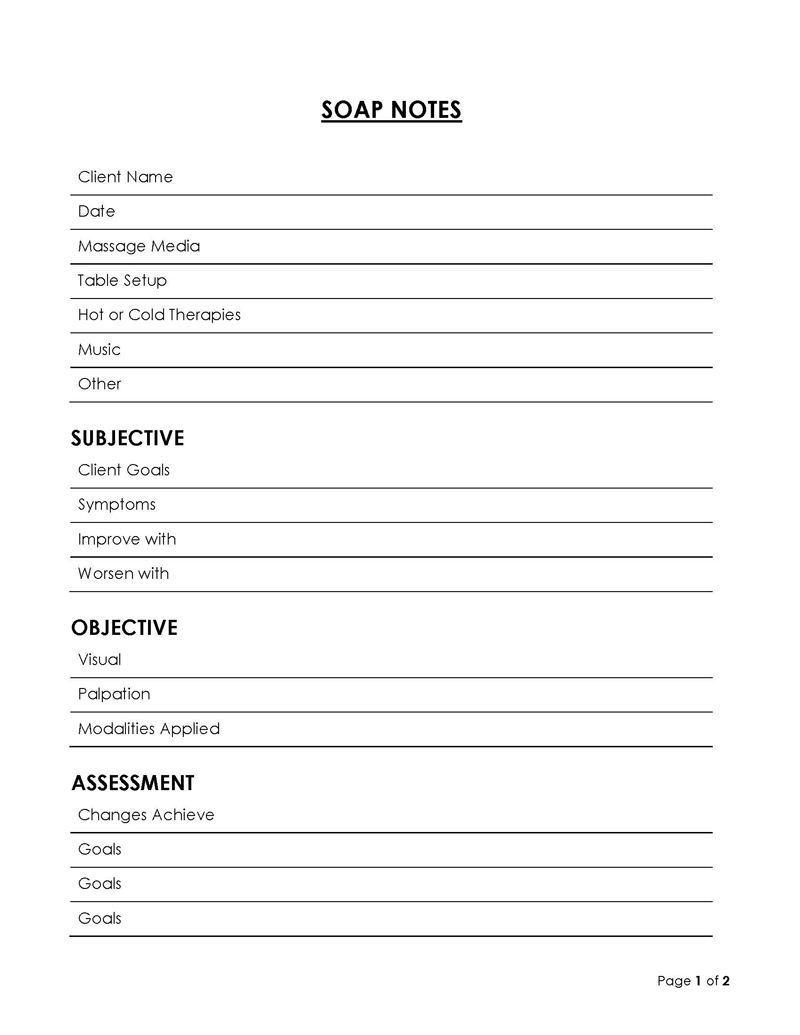
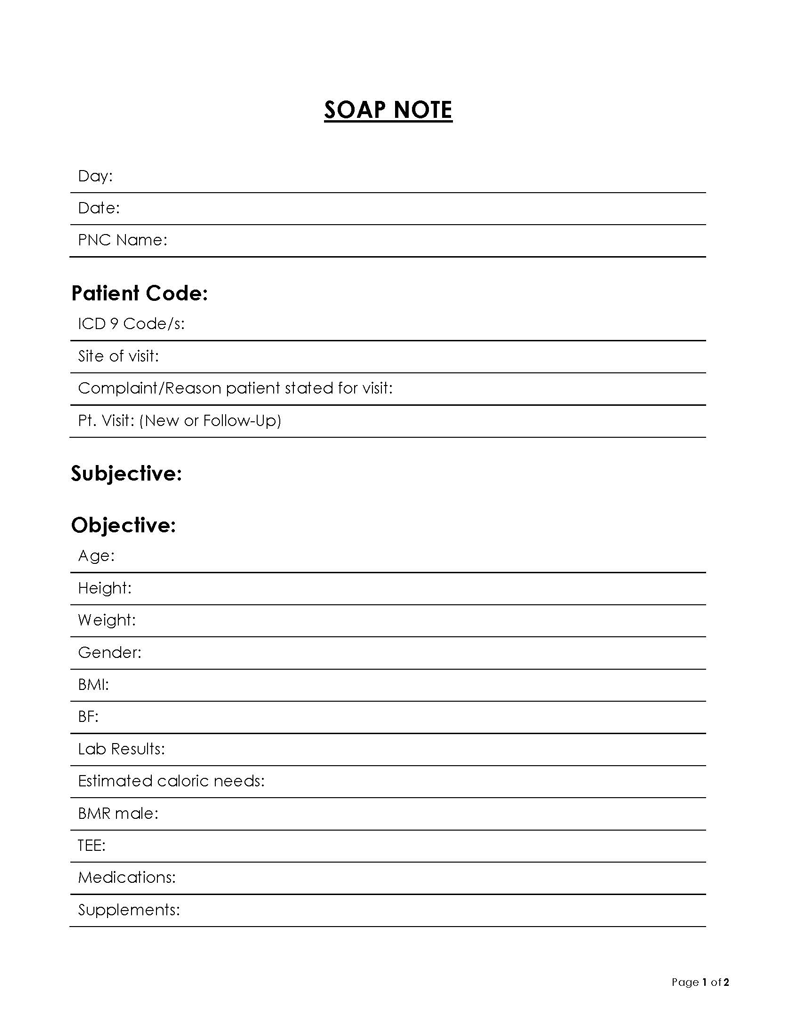
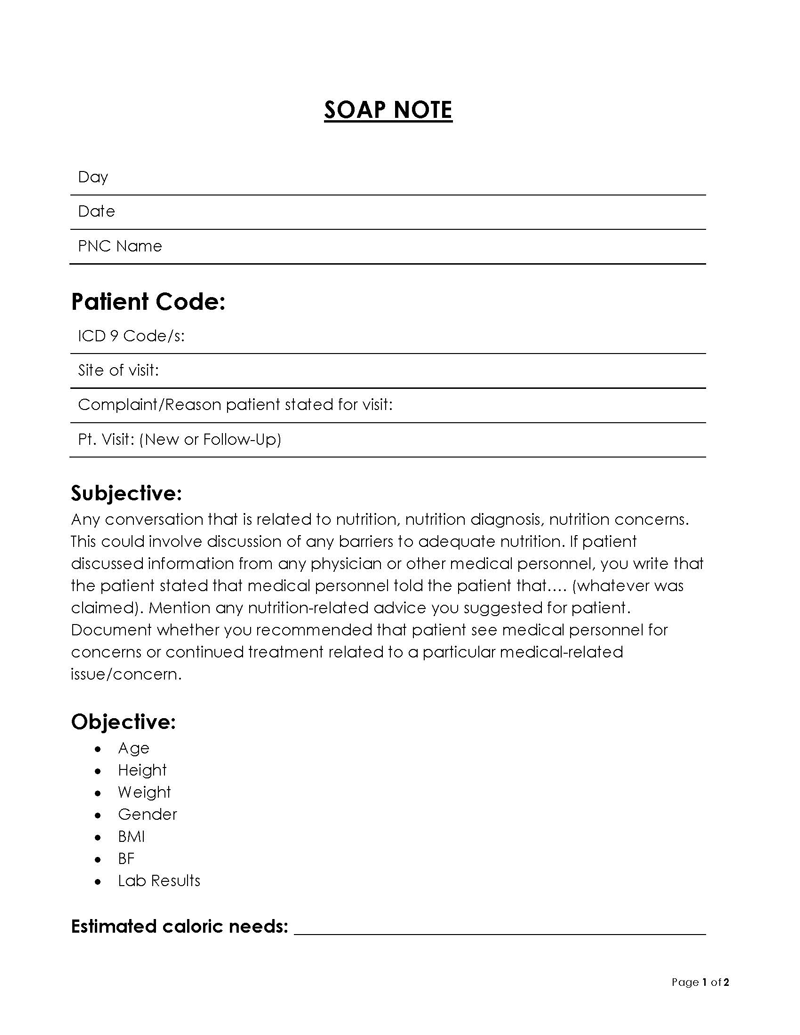
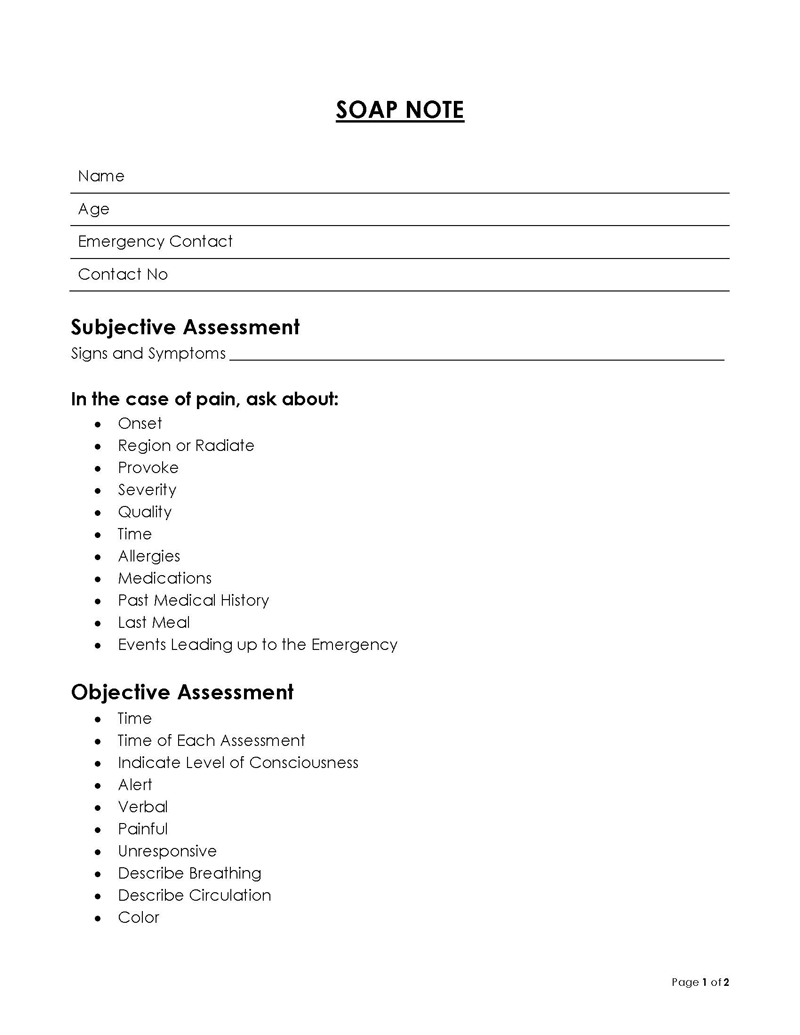
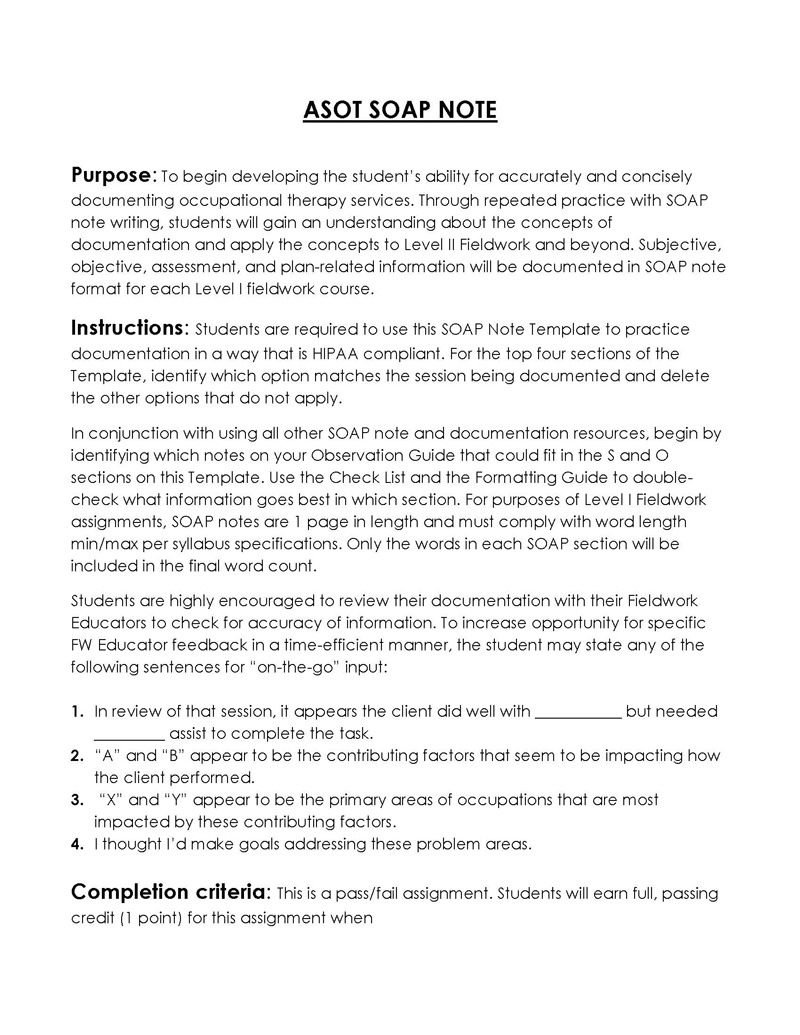
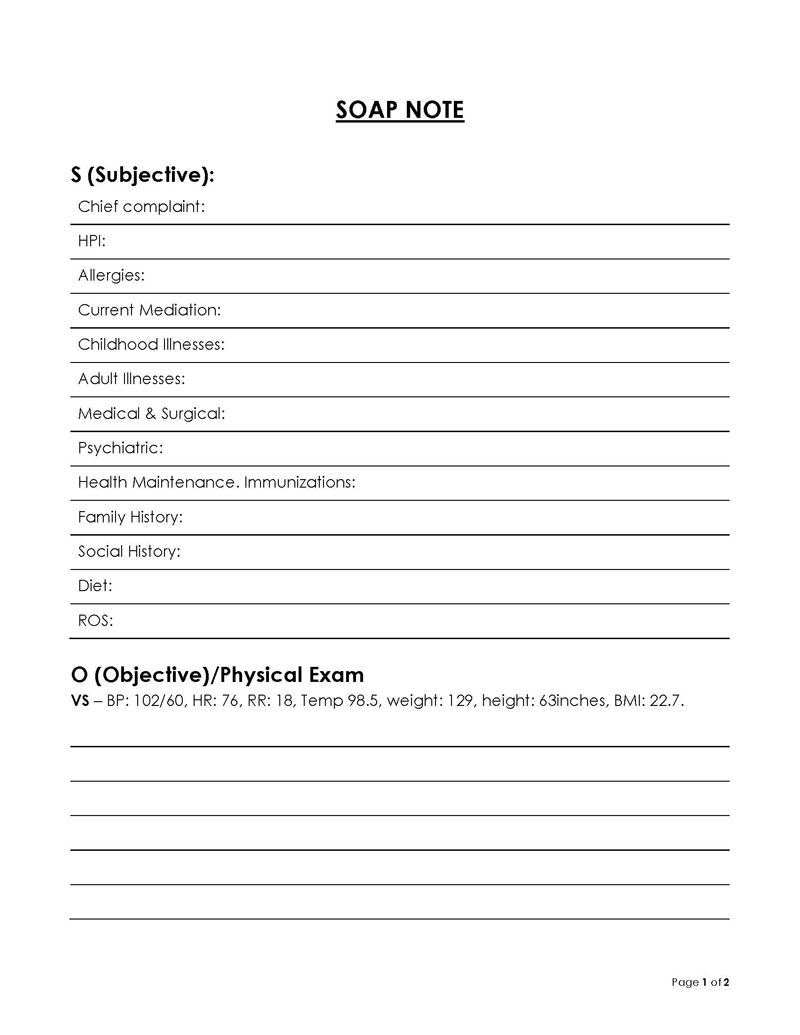
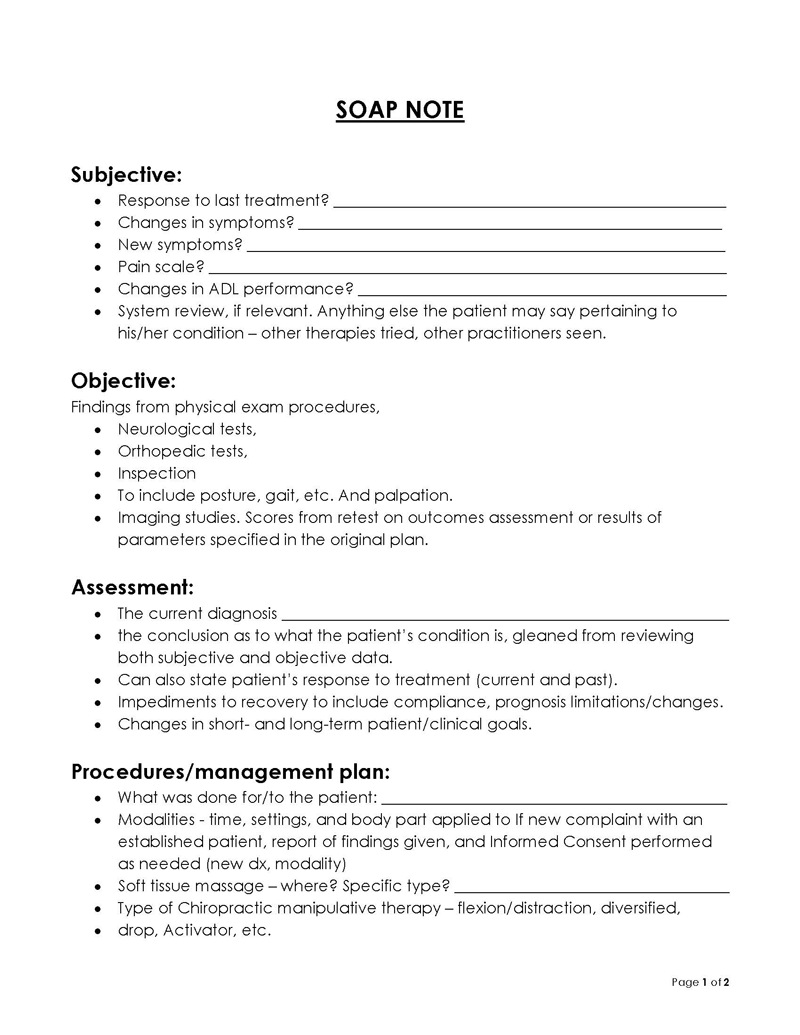
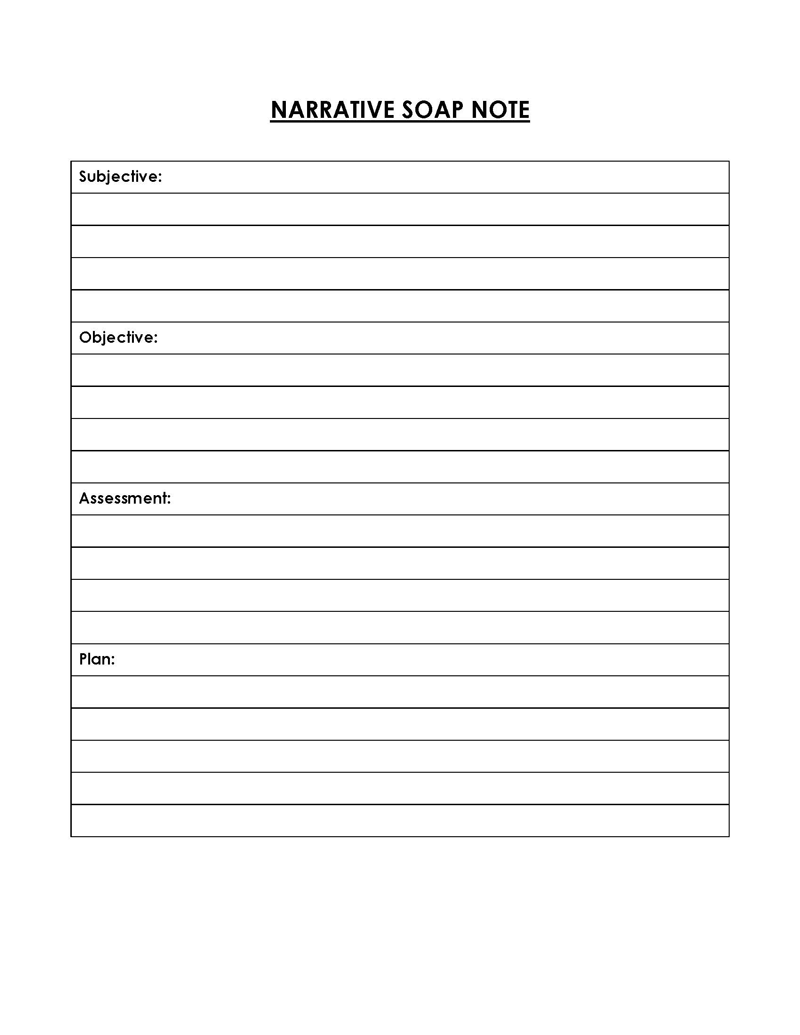
Free Templates
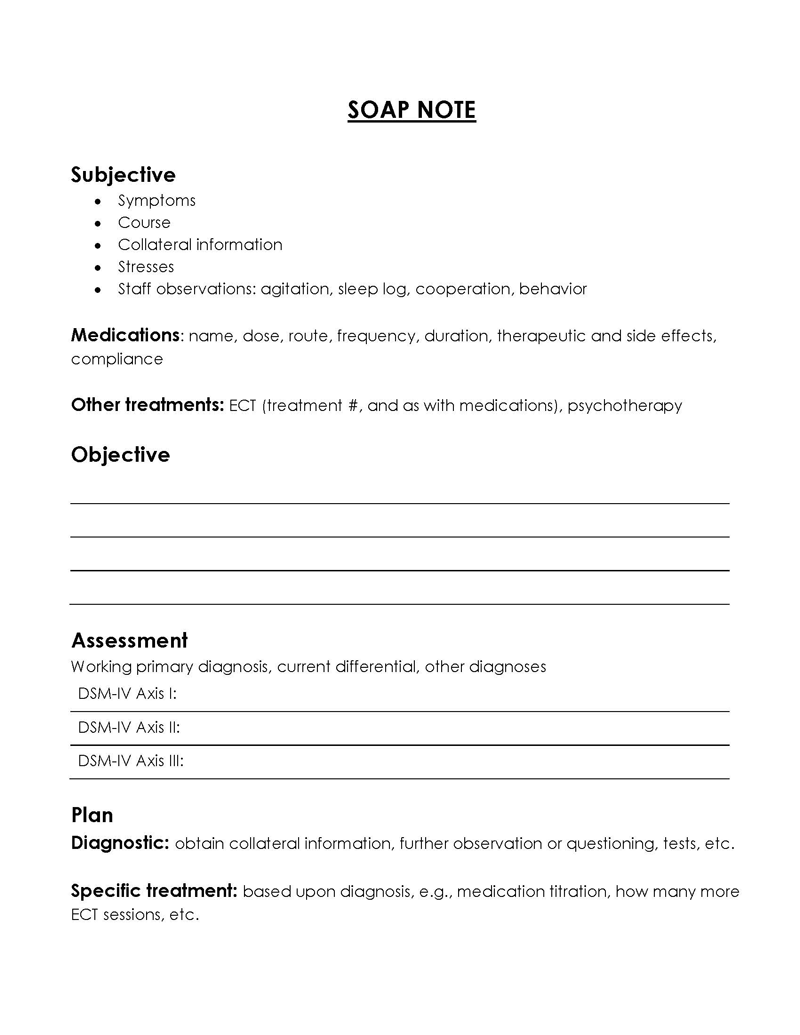
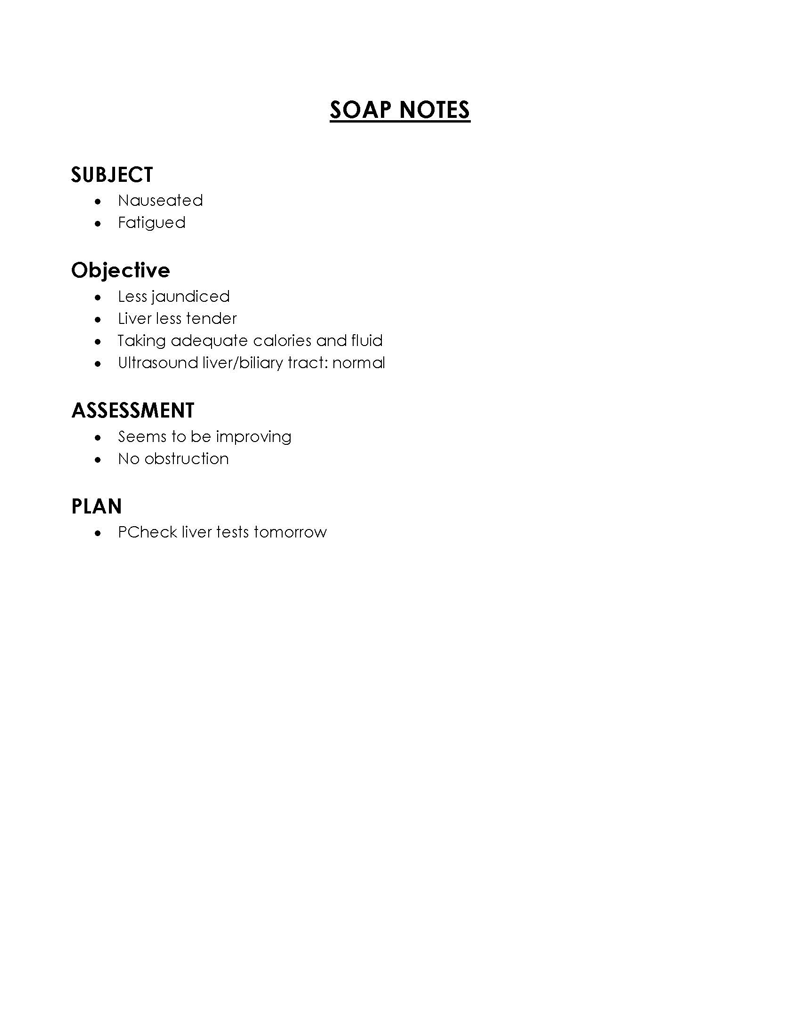
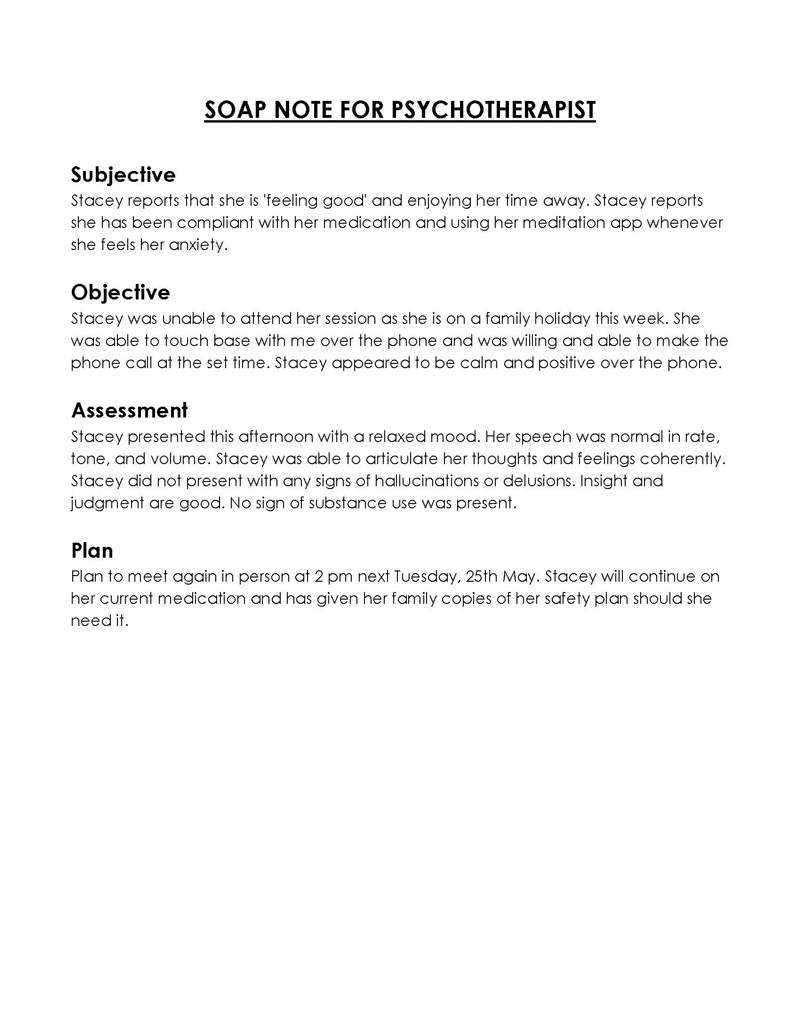
SOAP notes have several essential elements that you must include in them. Especially considering the legal credibility they entail. Inputting this information into these notes accurately can be a serious matter. Therefore, we suggest you utilize these free editable templates, which already contain the sections required to be filled for documenting your patients’ problems. Doing so can improve consistency and ensure accuracy in your notes.
Where SOAP Notes are Used
As mentioned briefly earlier, the notes have multiple uses in multiple different facets/fields of medicine apart from primary care or physical/medical specialty.
Some of these areas of fields include:
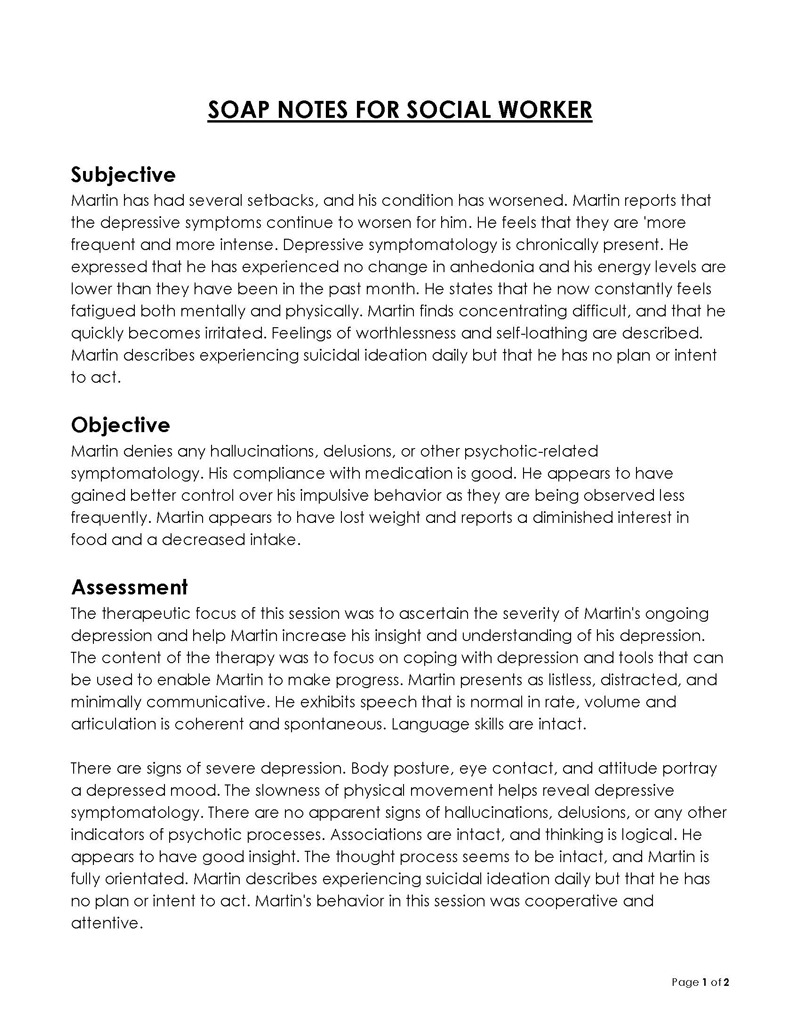
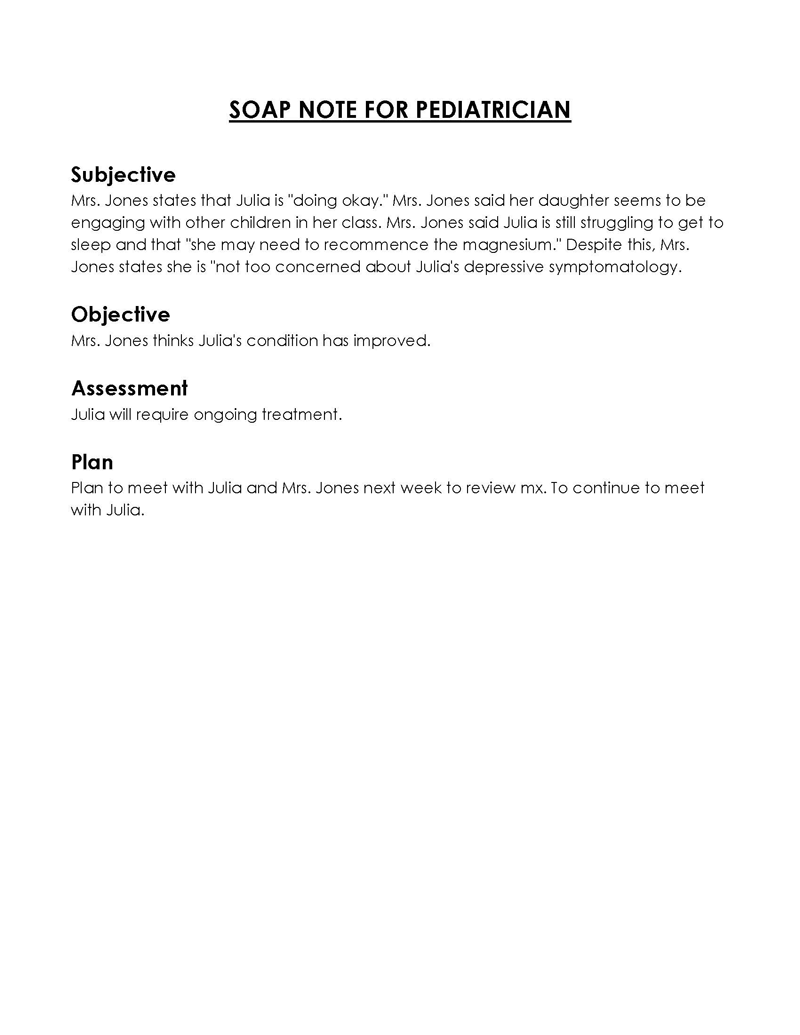
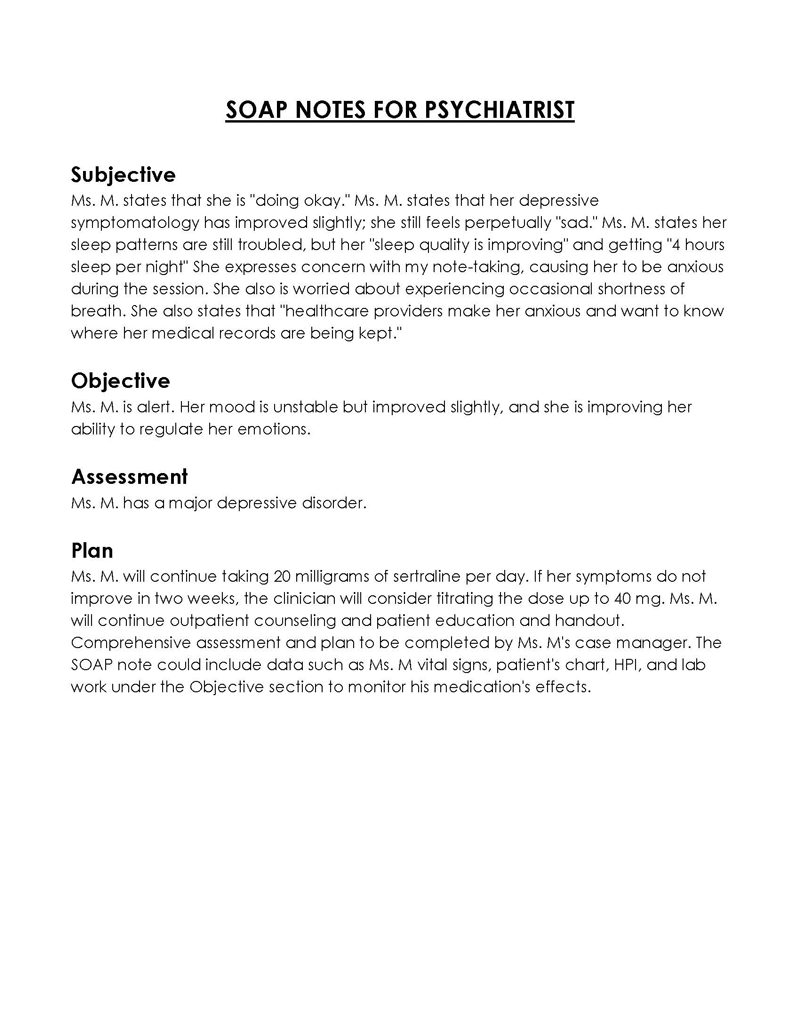
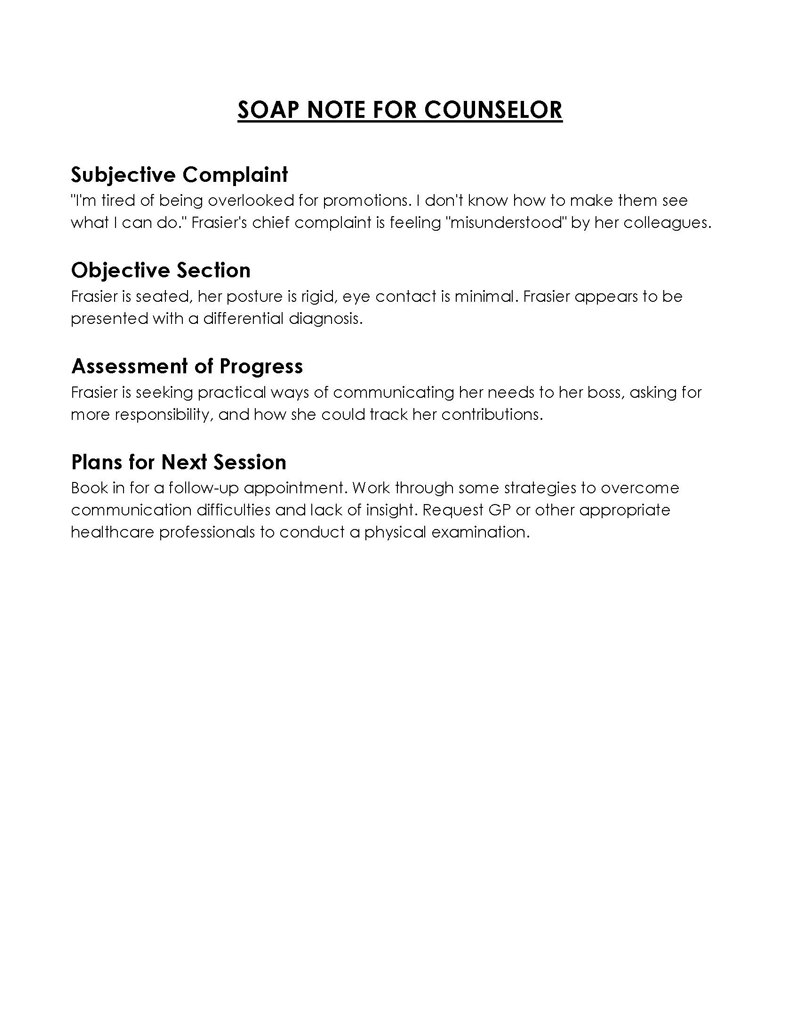
Psychiatry
They play a vital role in the treatment or therapy professionals in the field of psychology provide to their patients. Psychiatrists and therapists utilize these notes while documenting the patients’ problems and proceeding further with therapeutic or medical treatments. The notes of this type include information such as mental health evaluations, therapy sessions planning, and other prescribed treatment plans.
Obstetrics and gynecology
Similarly, these notes have significant importance in the practice of gynecology as well. The medical professionals in this field utilize them to document prenatal visits, labor and delivery, postpartum care and other gynecological examinations unrelated to pregnancy too. It helps provide ongoing treatment to soon-to-be mothers in a continual manner throughout their pregnancy and more.
Cardiology
They have special significance in the treatment healthcare professionals provide in the field of cardiology. They help document factors such as the ongoing cardiological conditions patients might have and keep track of the treatments to be administered on them.
For instance, a patient could have the problem of chest pains and/or palpitation. This will be documented in the subjective section, after which comes the objective section in which you can detail the factors such as blood pressure readings and ECG result details, etc. Based on these, you can proceed further towards the treatment plan for the patient suffering with cardiac issues.
Dermatology
Similar to the rest of the healthcare fields, the notes are widely utilized in the delivery of treatment for ongoing dermatological conditions too. Dermatologists essentially consider the subjective, objective, assessment and planning factors in the treatment plan they devise for their patients. For instance, a dermatologist treating a patient with ongoing eczema might essentially utilize these notes.
Long-term care providers
Medical professionals delivering long-term care or treatments to individuals residing in living facilities also benefit from the notes. For example, old age homes.
Commonly Used Abbreviations in a SOAP Note
For additional ease in notes-taking, healthcare professionals can utilize certain medical abbreviations in their notes. Doing so saves precious time and maintains the focus on the problem and its treatment.
Some of the abbreviations professionals or doctors usually use in these notes are:
- CC: chief complaint
- HPI: history of present illness
- PMH: past medical history
- PE: physical examination
- Dx: diagnosis
- DDx: differential diagnosis
- BP: blood pressure
- HR: heart rate
- Temp: temperature
- CBC: complete blood count
- Rx: prescription
- Tx: treatment
- Labs: lab tests
- CXR: chest x-ray
- RR: respiratory rate
- ECG: electrocardiogram
- SOB: shortness of breath
- NPO: nil per os (nothing by mouth)
- Ed: education
tip
Note that people can misunderstand abbreviations based on their conciseness and legibility factors. These are essential parts of the documentation process, therefore, use them with extra caution. Accidentally writing the wrong abbreviations, could result in medical issues for the patient and legal issues for you.
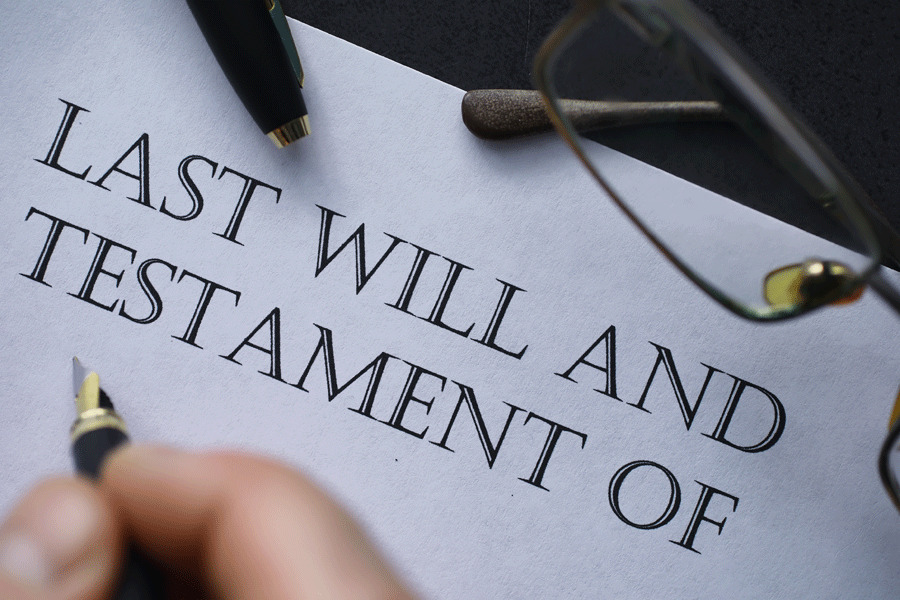
Legal Considerations of Using a SOAP Note
SOAP notes are medical documents that are directly related to the medical treatment individuals receive from you or at your medical facility. Therefore, they entail a certain level of legal liability. A person’s healthcare is directly concerned with their life, which is obviously a serious matter of concern.
You must consider factors such as the accuracy of documented data, applicable legal and regulatory requirements such as compliance of HIPAA in the United States, and obtaining patients’ informed consent while writing the notes to avoid potential legal complications. Informed consent is the consent you obtain from the patient in question pertaining to the administering of medical interventions for treatment.
Moreover, factors concerning the access, retention, and release of the data contained in these documents is equally essential. For instance, if the notes concerning a particular case are either not stored suitably, or released to some unrelated or unsuitable part(ies), it might cause the patient potential harm in a variety of manners.
Therefore, you are requested to consider all of the aforementioned factors in the process of using the notes.
Conclusion
SOAP notes are essential documents that medical professionals use in the process of treating their patients. SOAP stands for “subjective”, “objective”, “assessment,” and “plan”. Each of these 4 components entails a different category of information pertaining to the patients you treat. You can utilize them in multiple different areas of medical practice. For instance, in cardiology, psychiatry/psychology, gynecology and dermatology. These notes help ensure effective communication between healthcare professional teams, continuity of suitable medical treatment and improved consistency of medical treatments. Despite the conciseness and ease of usage of these notes, they have certain legal and ethical implications, which must be considered during their usage.